Worker Health and Safety from the Oil Rig to the Shoreline
June 23, 2010
Testimony Committee on Education and Labor U.S. House of Representatives
John Howard, M.D.
Director, National Institute for Occupational Safety and Health
Centers for Disease Control and Prevention
U.S. Department of Health and Human Services
Good morning, Mr. Chairman, Ranking Member Kline, and distinguished members of the committee. Thank you for inviting me to testify today. I am Dr. John Howard, Director of the National Institute for Occupational Safety and Health (NIOSH), which is part of the Centers for Disease Control and Prevention (CDC) within the U.S. Department of Health and Human Services (HHS). I am here today to provide an update on NIOSH′s response to the recent Gulf of Mexico oil spill and our ongoing efforts to anticipate, monitor and respond to the potential health threats to workers.
CDC′s Coordinated Response
On April 20, 2010, after the fire and explosion on the Deepwater Horizon leading to the oil spill, CDC immediately began monitoring the situation. On April 22, CDC staff participated in the National Response Team′s activation meeting and then formed an oil spill task force to monitor and respond to any potential public health hazards associated with the oil spill. CDC quickly publicized information describing the potential health risks associated with the oil spill and steps individuals can take to protect their health and safety. On May 10, CDC′s Emergency Operations Center (EOC) officially activated and began coordinating CDC′s response, which includes staff from NIOSH and the National Center for Environmental Health, which is leading the EOC incident command and response activities. As of June 17, 204 CDC staff were involved in the agency′s response to the oil spill, and many of these staff are from NIOSH.
Throughout the response to the oil spill, CDC has closely coordinated our efforts with other components of HHS – including the Assistant Secretary for Preparedness and Response, the Food and Drug Administration (FDA), the National Institutes of Health (NIH), and the Substance Abuse and Mental Health Services Administration; other federal partners like the U.S. Coast Guard (USCG), the Department of Labor′s Occupational Safety and Health Administration (OSHA), and the Environmental Protection Agency (EPA); and the Gulf coast states.
NIOSH′s Response Activities
As part of CDC′s overall response, NIOSH involvement in the oil spill response began very early. NIOSH was with OSHA and NIH′s National Institute of Environmental Health Sciences (NIEHS) in the initial HHS response visit to the Gulf during the week of May 3. Since then, NIOSH has been providing information to BP, OSHA, the Coast Guard, and other federal and state partners about protecting response workers and volunteers from potential occupational safety and health hazards. I would now like to provide an update on the work that NIOSH has been doing to protect the response workers and volunteers, which includes:
- Rostering responders;
- Collecting and evaluating health surveillance and injury and illness data;
- Conducting a health hazard evaluation of workers;
- Developing recommendations for response workers and volunteers; and
- Providing guidance on traumatic incident stress.
Rostering Responders
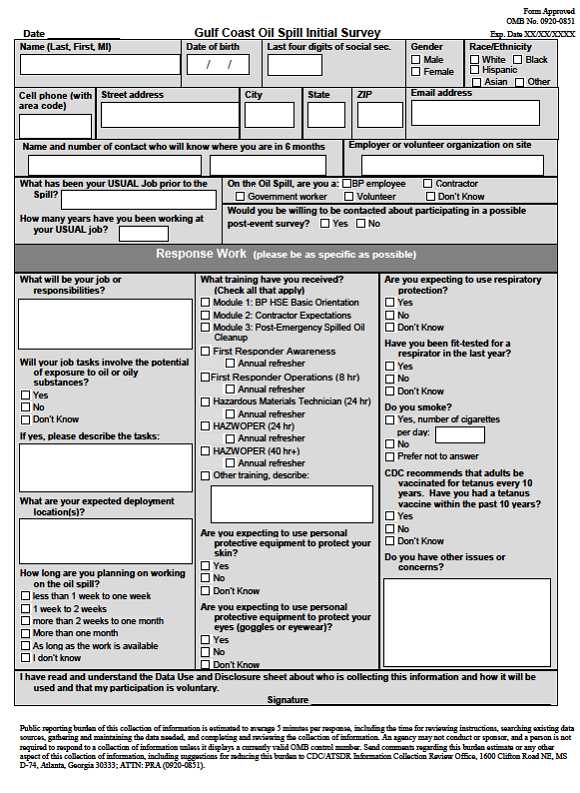
NIOSH is administering surveys to thousands of clean-up workers in an effort to compile a roster that will serve as an accurate record of many individuals involved in the response. The information collected in this roster would be vital for possible future studies to determine whether health conditions that may develop in the future are associated with occupational exposures during the cleanup. A roster is an important tool to capture site-specific information, such as a worker′s job task, time on task, available exposure information, use of personal protective equipment (PPE), and other related factors. Participation in the survey is voluntary, and once the information is collected, NIOSH will protect individuals′ personally identifiable information as confidential to the extent allowed by the law.We are rostering workers as they complete safety training required for all responders and at the staging areas in order to reach workers already trained. It has been challenging to enroll workers due to the different locations staging areas and training sites. To date we have visited many of the staging areas in Louisiana to roster workers. We are currently enrolling workers in Mississippi, Alabama, and Florida and returning to LA′s newly added staging areas. New staging areas are continuously being added in locations across the Gulf region. Through our rostering efforts, we have already captured information from more than 14,000 workers responding to this event. In an attempt to reach all cleanup workers, the survey is being administered in English, Spanish, and Vietnamese. This is an unprecedented effort, and NIOSH is working hard to ensure that our roster will include information for as many of the responders to this event as possible.
In the last week, NIOSH also began rostering response workers online through a secure Website. NIOSH has provided the secure link to multiple federal agencies and BP, and has asked them to refer workers to the Website to complete the rostering form electronically. NIOSH is also reaching out to state and local partners to identify mechanisms to assist us in rostering all parish, local, state, and National Guard workers. NIOSH has created a database, which includes information from the paper surveys that is entered manually as well as information uploaded electronically from the Web-based surveys. Data from the electronic survey will be analyzed in the same manner as those completed on paper. A copy of the survey is included as Exhibit 1.
Collecting and Evaluating Health Surveillance and Injury and Illness Data
CDC is conducting surveillance across the Gulf States for health effects possibly related to the oil spill using national and state-based surveillance systems. NIOSH is analyzing injury and illness data collected at the BP medical sites. NIOSH is using all of this data to monitor reports of worker illness and injury and to work with the States, OSHA, and BP to identify trends and potential health effects. CDC′s National Center for Environmental Health (NCEH) contacted the American Association of Poison Control Centers to request that local poison control centers code any calls related to the oil spill so that CDC can track them. The majority of the calls we have received so far have been from response workers. NIOSH is also using CDC′s BioSense surveillance system – which analyzes diagnostic and pre-diagnostic health data from clinical laboratories, hospital systems, ambulatory care sites, health plans, U.S. Department of Defense and Veterans Administration medical treatment facilities, and pharmacy chains – to enhance surveillance for respiratory health effects in states along the Gulf of Mexico coast. CDC is receiving surveillance data collected by Alabama, Florida, Louisiana and Mississippi and is working closely with the respective state epidemiologists to look for any health effects that may be related to the oil spill. CDC posted results from these collaborative surveillance activities on the CDC Website on June 10. NIOSH is also encouraging workers to report symptoms they feel are associated with response work to employers, medical personnel, or state and local health departments.
Conducting Health Hazard Evaluation of Workers
NIOSH has a unique opportunity to assess these occupational safety and health hazards that may arise as we conduct Health Hazard Evaluations (HHEs) of reported illnesses among workers involved in onshore and offshore cleanup operations. Several NIOSH staff members have been deployed to the Gulf coast to work on the HHEs, including industrial hygienists – who are assessing exposures through observation, industrial hygiene assessments, and evaluation of work practices and use of PPE – and medical officers – who are evaluating illnesses and injuries among groups of onshore and offshore workers. Industrial hygienists are evaluating exposures to volatile organic compounds such as carbon monoxide, hydrogen sulfide, benzene, diesel exhaust, and propylene glycol (a component of the dispersant). The medical teams are administering health symptom surveys to workers involved in various onshore and offshore operations. The Louisiana Department of Health and Hospitals has agreed to provide medical reports of seven previously hospitalized fishermen for NIOSH physicians to review. Additional reports of the incident from the Coast Guard, OSHA, and BP are being reviewed as well. Once the HHE is completed, NIOSH will compile the findings and recommendations in a report that will be provided to employer and employee representatives, and it will be publicly available on the NIOSH Website.
The additional HHE request received on June 18 will assist NIOSH in addressing activities associated with exposures that may occur during all types of operations related to this event. Since knowledge about potential inhalational exposures to the mixed exposure of crude oil, dispersant and combustion products associated with the Deepwater Horizon response work is incomplete and still evolving, NIOSH believes it is prudent to reduce the potential for adverse health effects by the responsible use of engineering controls, administrative controls and PPE, including respirators when appropriate. The following is a description of each of the categories of worker exposure.
- Source Control Activities: The source control vessels conduct activities closest to the area where crude oil appears on the surface, including drilling relief wells, conducting underwater operations at the source such as subsurface dispersant application, and providing support and supplies.
- Vessels involved in Burning Crude Oil: Vessels involved in crude oil burning are exposed to crude oil/dispersant that is less aged and may emit more VOCs than crude/dispersant closer to shore that may have undergone more weathering.
- Vessels not involved in Source Control or Burning: Some vessels operating off-shore engage in deployment of containment and sorbent booms and skimming operations to remove oil from the water. These vessels are not involved in burning nor are they located in close proximity to in-situ burning. Generally, these vessels have contact with oil that has weathered, and, as such, does not emit significant amounts of VOCs
- Shoreline Activities: The types of activities associated with shoreline cleaning include manual removal of “tarballs” or “tarpatties,” shovel removal of oiled-contaminated sand, low pressure flushing, manual sorbent application, and manual cutting of vegetation.
- Decontamination Activities: Vessels, PPE and other equipment may become contaminated with weathered oil. Workers and volunteers may also be involved in cleaning and caring for birds, turtles and other wildlife
- Waste Stream Management Activities: Response and remediation workers are engaged in the disposal and recycling of hazardous solid and liquid wastes during collection, storage, transport and final disposal.
Health Studies of Tanker Oil Spills
It is important to note that in recent years several studies of previous oil spill response efforts have reported acute health effects in response workers. These studies may underestimate the health effects associated with oil response work since the magnitude and duration of the Deepwater Horizon response is unprecedented. At this time, there has been no comprehensive assessment of all response worksites in the Gulf, and as a result, we have an incomplete understanding of the human health toxicity associated with exposure to large amounts of dispersants and the toxicity associated with mixed exposure to large amounts of crude oil and dispersants together. This means that knowledge about potential human health effects to the mixed exposure of crude oil and dispersant associated with the Deepwater Horizon response work is still evolving. Therefore, NIOSH believes it is prudent to reduce the potential for such adverse health effects by the responsible use of administrative controls and PPE.Developing Recommendations for Response Workers and Volunteers
To ensure a comprehensive approach to worker safety and health, NIOSH has been working closely with OSHA to develop Interim Guidance which focuses on issues specific to the Deepwater Horizon response. The recommendations in the Interim Guidance include:- Conducting exposure assessment: Exposures to toxic chemical and physical agents should be comprehensively and routinely assessed during work activities under varying conditions.
- Pre-Placement Evaluation: NIOSH currently is working with OSHA to develop recommendations for pre-placement evaluations for workers involved in the Deepwater Horizon response to ensure that each worker receives appropriate advice about his or her health status and the potential demands of the work before they begin.
- Medical Care and Symptom, Near-Miss, Injury and Illness Reporting and Recording: All health symptoms, illnesses, injuries or near-misses related to work activities should be reported by workers and volunteers, should be recorded by employers, contractors and volunteer organizations, and should be evaluated by safety and health or licensed health care professionals with action taken to protect workers
- Heat stress prevention: Excessive exposure to hot environments can cause a variety of heat-related problems, including heat stroke, heat exhaustion, heat cramps, and fainting. Heat can also increase the risk of injuries in workers from sweaty palms, fogged-up safety eyewear, and dizziness. Protective clothing and other PPE will increase the risk of heat-related problems. PPE should be selected to minimize heat stress on the wearer.
- Fatigue Prevention: Disaster response workers often work longer shifts and more consecutive shifts than the typical 40-hour work week. Working longer hours may increase the risk of work injuries and accidents and can contribute to poor health. Therefore, disaster response organizations should have management plans in place to minimize fatigue risks, recognize hazards, and provide regular opportunities for worker rest and recovery.
- Use of PPE: A variety of PPE will be needed by Deepwater Horizon response workers and volunteers. Administrative controls and engineering controls should be utilized first to minimize the need for PPE in any particular job. Where such controls will not effectively minimize the exposures, then PPE will be necessary.
- Guidance on Selection of Protective Clothing: Choosing the proper chemical and flame resistant protective garments is an exercise in the selection of fabric, seam and design. The selection must be based on expected exposure and verified by field audits and changed if the selected PPE does not perform adequately. The potential for contribution to heat stress must also be considered in the selection of protective clothing, in addition to the potential exposure to fire, water, oil and tar, and other chemicals.
- Reuse of Personal Protective Equipment: Consult the manufacturer′s instructions on whether personal protective equipment should be disposed of or cleaned after use. Many manufacturers of PPE, in particular manufacturers of gloves, will provide information on breakthrough times from various chemicals (time it takes for the chemical to pass through the protective material). Given the warm and humid conditions existing during the Deepwater Horizon Response, disposable filtering facepiece respirators will likely need to be discarded after several hours of use, in part because they will become moist with perspiration.
- Use of Respiratory Protection: A decision to use respiratory protection should be based on the best available qualitative information using the expert opinion method and on the best available comprehensive quantitative information about the type and level of exposure to toxic chemical and physical agents by the inhalational route. The use of effective engineering and administrative controls, and other personal protective equipment should be implemented before the use of respirators for worker protection is considered.
- Resources for Use of Respiratory Protection: Information about which respirators are approved by NIOSH, how to get them and how to use them, can be found at the NIOSH Respirator Trusted-Source Information Page at: http://www.cdc.gov/niosh/npptl/topics/respirators/disp_part/RespSource.html#sect1.
- Voluntary Use of Respirators: Respiratory protection may be worn by employees voluntarily as permitted by the OSHA Respiratory Protection Standard (29 CFR Section 1910.134). An employer may provide respirators at employees′ requests or permit employees to use their own respirators if the employer determines that use, in itself, will not create a hazard (29 CFR Section 1910.134(c)(2)(i)).
Recommendations contained in the Interim Guidance will be updated as more information about exposures is collected and assessed in relationship to the incidence and prevalence of symptoms, illnesses and injuries.
Providing Guidance on Traumatic Incident Stress
Deepwater Horizon response workers and volunteers are at risk of feeling uncomfortable levels of stress from what mental health professionals refer to as a traumatic incident. NIOSH is developing guidance that describes the range of ordinary reactions to stress – such as complaints of physical ailments, trouble thinking clearly, emotional concerns, and behavioral changes – which responders may experience during their work or in the weeks or months that follow. NIOSH guidance recommends that responders take care of themselves and monitor their own emotional and physical health both during the response and after the event ends. Specifically, responders should: control the pace of their rescue and recovery efforts and be mindful of potential hazards; maintain adequate nutrition, hydration and rest; and monitor their own mental and emotional health. Additionally, the Substance Abuse and Mental Health Services Administration (SAMHSA) supports Mental Health First Aid training and other psychological health programs for dealing with trauma and stress for first responders, behavioral health workers, and persons who are experiencing the aftermath of traumatic situations. NIOSH and SAMHSA are collaborating to assure that the guidance provided is aligned with the tools and services available to individuals to address their reaction to this traumatic incident.
Conclusion
CDC continues to work diligently to anticipate, monitor and respond to potential health threats to protect the health and safety of workers, volunteers and residents along the Gulf coast. This oil spill underscores the importance of CDC′s work and the need for further health and safety research. It is important to protect response workers, volunteers and Gulf coast residents against potential health hazards now so that we can prevent future chronic health effects associated with this spill. As this event evolves and we learn more about potential health hazards, CDC will update our recommendations. I appreciate the opportunity to describe the steps NIOSH is taking to protect response workers and volunteers along the Gulf coast. Thank you for your continued support. I am pleased to answer any questions you may have.
Exhibit 1 – Gulf Coast Oil Spill Survey
- Page last reviewed: July 1, 2010
- Page last updated: July 1, 2010
- Content source:




 ShareCompartir
ShareCompartir