Opioid Prescribing
Where you live matters
Overview
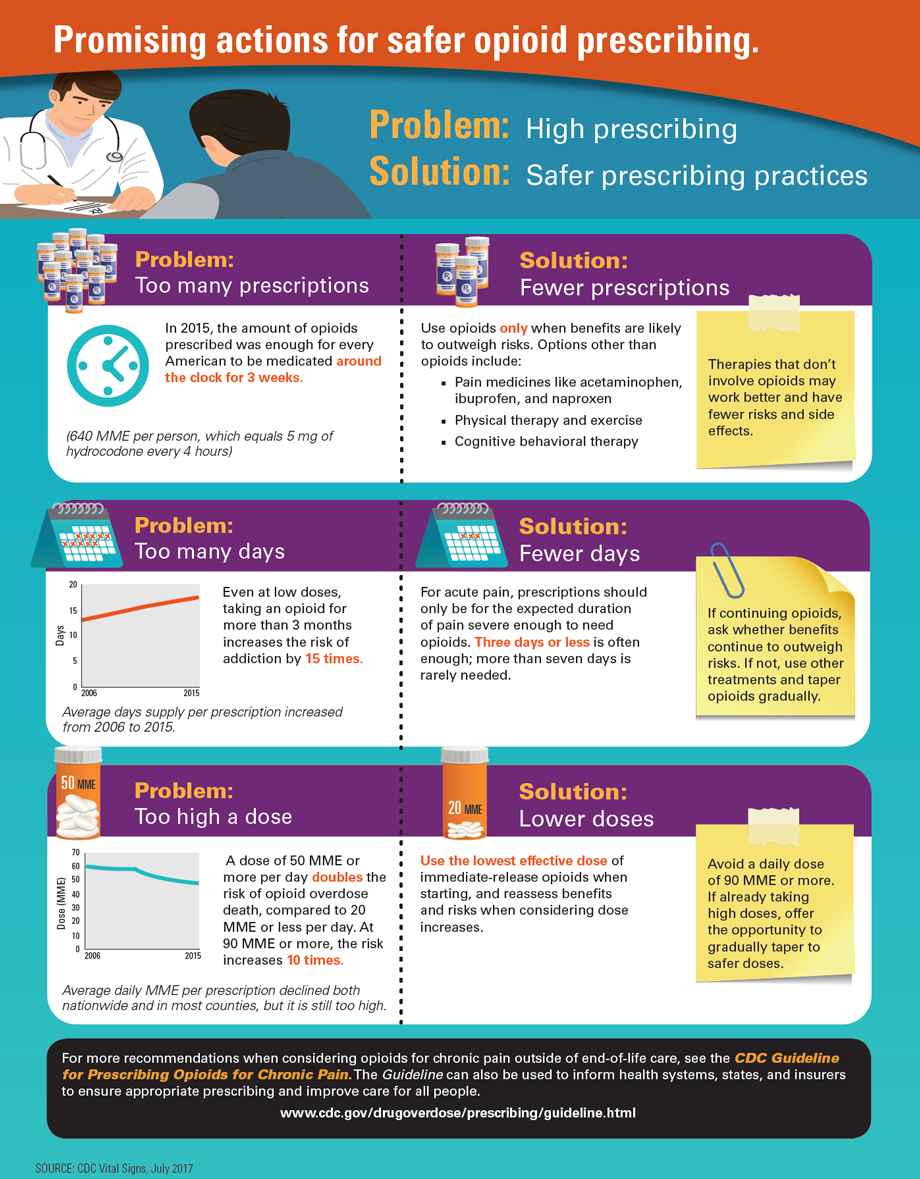
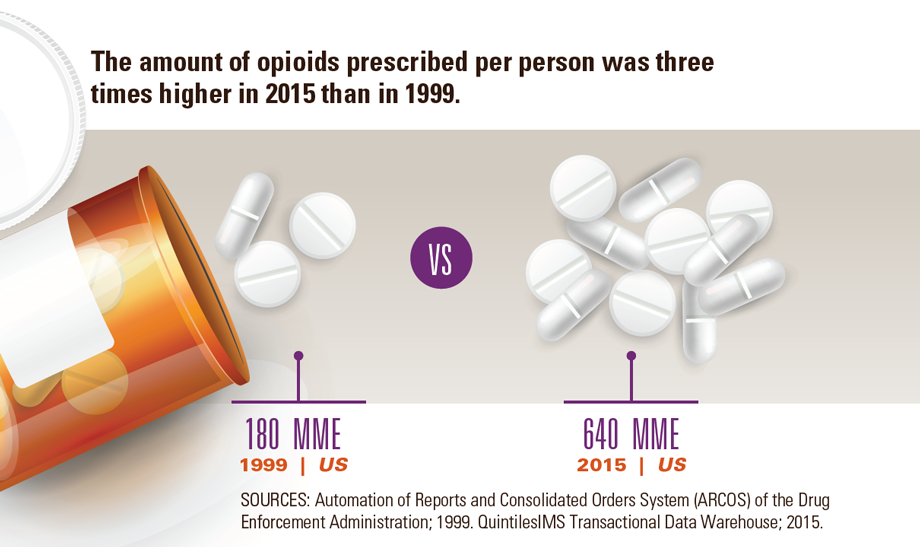
The amount of opioids prescribed in the US peaked in 2010 and then decreased each year through 2015. However, prescribing remains high and vary widely from county to county. Healthcare providers began using opioids in the late 1990s to treat chronic pain (not related to cancer), such as arthritis and back pain. As this continued, more opioid prescriptions were written, for more days per prescription, in higher doses. Taking opioids for longer periods of time or in higher doses increases the risk of addiction, overdose, and death. In 2015, six times more opioids per resident were dispensed in the highest-prescribing counties than in the lowest-prescribing counties. County-level characteristics, such as rural versus urban, income level, and demographics, only explained about a third of the differences. This suggests that people receive different care depending on where they live. Healthcare providers have an important role in offering safer and more effective pain treatment.
Healthcare providers can:
- Follow the CDC Guideline for Prescribing Opioids for Chronic Pain, which includes recommendations such as:
- Use opioids only when benefits are likely to outweigh risks.
- Start with the lowest effective dose of immediate-release opioids. For acute pain, prescribe only the number of days that the pain is expected to be severe enough to require opioids.
- Reassess benefits and risks if considering dose increases.
- Use state-based prescription drug monitoring programs (PDMPs) which help identify patients at risk of addiction or overdose.

Providers in the highest prescribing counties prescribed 6 times more opioids per person than the lowest prescribing counties in 2015.
Half of US counties had a decrease in the amount of opioids (MME*) prescribed per person from 2010 to 2015.
The MME prescribed per person in 2015 was about 3 times as high as in 1999.
* MME, morphine milligram equivalents, is a way to calculate the total amount of opioids, accounting for differences in opioid drug type and strength.
Problem
Despite recent declines, opioid prescribing is still high and inconsistent across the US.
View large image and text description
Some characteristics of counties with higher opioid prescribing:
- Small cities or large towns
- Higher percent of white residents
- More dentists and primary care physicians
- More people who are uninsured or unemployed
- More people who have diabetes, arthritis, or disability
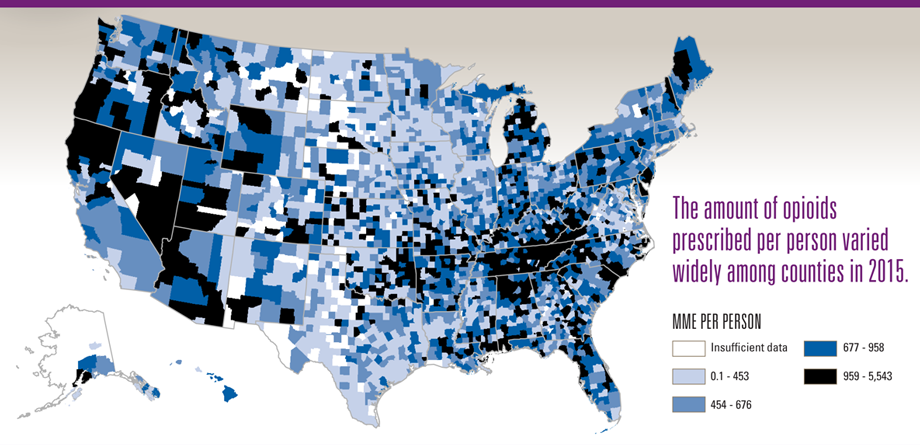
Higher opioid prescribing puts patients at risk for addiction and overdose. The wide variation among counties suggests a lack of consistency among providers when prescribing opioids. The CDC Guideline for Prescribing Opioids for Chronic Pain offers recommendations that may help to improve prescribing practices and ensure all patients receive safer, more effective pain treatment.
SOURCE: CDC Vital Signs, July 2017
What Can Be Done
The Federal Government is
- Educating healthcare providers and the public about pain management, addiction, and opioid overdose and providing guidance on safe and effective pain management.
- Equipping states with resources to implement and evaluate safe prescribing practices.
- Improving access to addiction treatment and recovery services.
- Increasing access to overdose-reversing drugs, such as naloxone.
- Tracking opioid-related trends to better understand and respond to the epidemic.
- Supporting cutting-edge research about pain management and addiction.
States can
- Maximize prescription drug monitoring programs (PDMPs) by using near real-time data reporting, integrating with electronic health records, and promoting routine provider use.
- Implement and evaluate programs to improve prescribing practices.
- Use data to identify and address high-risk prescribing.
- Enhance the use of prescribing guidelines based on the best available science.
- Increase access to medication-assisted treatment for addiction and naloxone for opioid overdose.
Health insurers can
- Refer to the Guideline in setting up prescription claims review programs to identify and address improper prescribing and use of opioids.
- Increase coverage for other proven treatments to reduce pain, such as physical therapy and non-opioid pain medicines.
- Cover clinicians’ time when they are conducting activities that improve quality and safety of pain management and addressing addiction. These can include patient counseling, coordination of care, and checking the patient’s prescription history in the PDMP.
- Reduce barriers (such as prior authorization) to use of nonopioid pain medications and medication-assisted treatment for addiction.
Healthcare providers can
- Follow the CDC Guideline for Prescribing Opioids for Chronic Pain, which includes recommendations such as:
- Use opioids only when benefits are likely to outweigh risks.
- Start with the lowest effective dose of immediate-release opioids. For acute pain, prescribe only the number of days that the pain is expected to be severe enough to require opioids.
- Reassess benefits and risks if considering dose increases.
- Use state-based PDMPs which help identify patients at risk of addiction or overdose.
Everyone can
- Consider non-opioid options for pain management.
- Store prescription opioids in a secure place, out of reach of others (including children, family, friends, and visitors).
- Dispose of medications properly as soon as the course of treatment is done. For more information, visit FDA at: http://www.fda.gov/Drugs/ResourcesForYou.
- Get help if you’re having trouble controlling your opioid use, SAMHSA’s National Helpline:
1-800-662-HELP.
Issue Details
- Vital Signs Issue details: Opioid Prescribing, Morbidity and Mortality Weekly Report (MMWR)
- Vital Signs – Opioid Prescribing [PODCAST – 1:15 minutes]
- Vital Signs – Opioid Prescribing [PSA – 0:60 seconds]
- CDC News Room – Digital Press Kit: Prescribing Opioids
- Morbidity and Mortality Weekly Report (MMWR): Vital Signs: Changes in Opioid Prescribing in the United States, 2006-2015
- Vital Signs, 2015: Today’s Heroin Epidemic: More People at Risk, Multiple Drugs Abused
- CDC Opioid Overdose Website
- CDC Guideline for Prescribing Opioids for Chronic Pain — United States, 2016
- CDC Learning Connection: Hot Training Topic
- Free Continuing Education (CE) on Opioid Prescribing (MMWR/Medscape)
- MedlinePlus – Prescription Drug Abuse
- MedlinePlus – Pain Relievers
- U.S. Department of Health & Human Services Strategy for Fighting Opioid Crisis
- JAMA Viewpoint
- Free Continuing Education (CE) on Opioid Prescribing (MMWR/Medscape)
- PDMP Center of Excellence, Brandeis University
- JAMA Special Communication: CDC Guideline for Prescribing Opioids for Chronic Pain
- Providers’ Clinical Support System for Medication Assisted Treatment
- Providers’ Clinical Support System for Opioid Therapies
- Office of the National Coordinator for Health Information Technology (ONC) – Linking PDMPs to Health IT
- National Alliance for Model State Drug Laws
- Page last reviewed: July 6, 2017
- Page last updated: September 26, 2017
- Content source:


 ShareCompartir
ShareCompartir