Blood Pressure Control
Helping Patients Take Their Medicine
On This Page
Overview
High blood pressure can lead to heart disease, stroke, kidney disease, and death. About 70% of US adults age 65 or older have high blood pressure and only about half have it under control (less than 140/90 mmHg). Blood pressure medicine (along with a healthy diet and exercise) can protect the heart, brain, and kidneys, but only if patients take it and keep their blood pressure controlled. However, at least 25% of adults, ages 65 or older, with Medicare Part D prescription drug insurance are not taking their blood pressure medicine as directed. This means they may skip doses or stop taking it altogether. Health care systems, including providers, medical practices, pharmacies, hospitals, community health workers, and insurers can work with patients to make taking medicine easier.
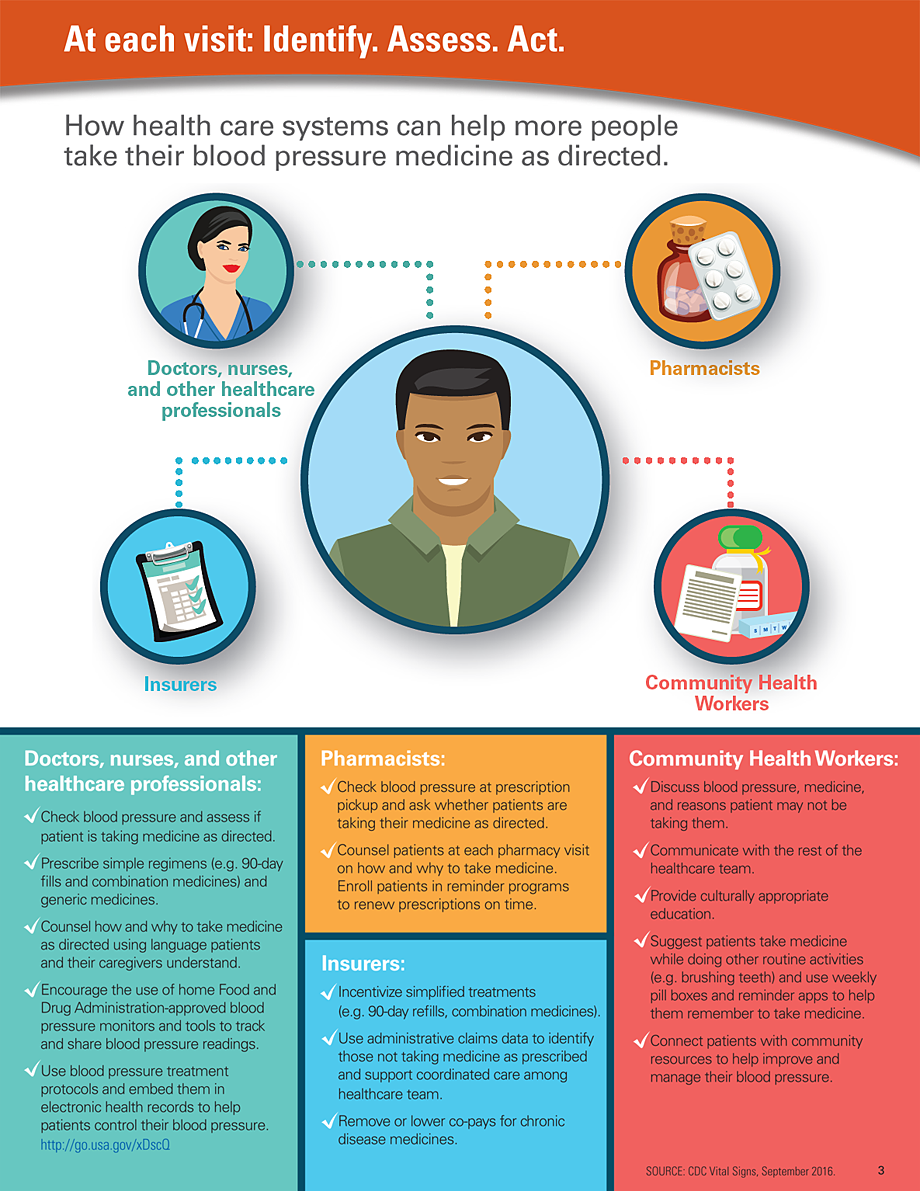
Health care systems can:
- Simplify blood pressure treatment (e.g. prescribe 90-day refills and combination medicines and coordinate pill refills for the same date) and prescribe generic medicines.
- Involve the entire healthcare team at several points of care to ensure patients are taking medicine as directed and to address patient concerns about side effects. Implement effective blood pressure treatment protocols in clinical practice. http://go.usa.gov/xjf59
- Encourage the use of home blood pressure monitors and easy-to-use tools (e.g. blood pressure logs and mobile apps) to track and share blood pressure readings.
- Address financial barriers, such as high co-pays and deductibles.
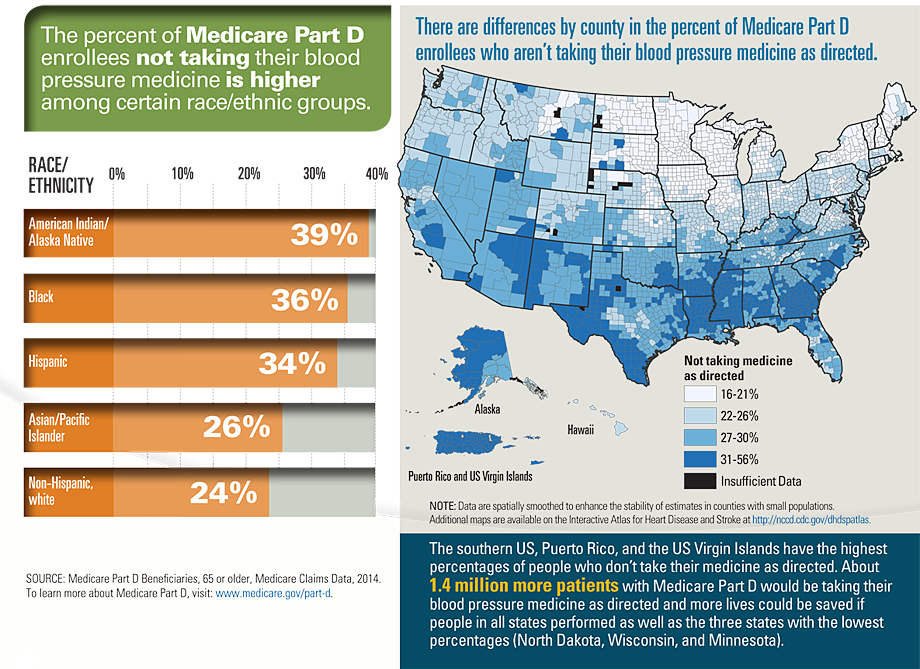
About 70% of US adults, ages 65 or older, have high blood pressure.
Nearly 50% of adults ages 65 or older with high blood pressure don’t have it under control.
About 5 million adults, ages 65 or older, with Medicare Part D aren’t taking their blood pressure medicine as directed.
Problem
Medicines don’t work if people don’t take them.
The reasons people don’t take their blood pressure medicine as directed vary:
- Not filling the prescription – Nearly 25% of new prescriptions for blood pressure medicine are never filled.
- No symptoms – People with high blood pressure often don’t have symptoms so some may not treat a problem they don’t notice.
- Complexity – People don’t know when to take which pills when they have multiple medicines.
- Side effects – Medicines may have unwanted side effects.
- Forgetting – People forget to take their medicine or refill prescriptions on time.
- Cost – Medicine costs may be too high for some people.
Infographic
What Can Be Done
The Federal government is
- Leading the national Million Hearts® initiative where public health and health care systems work together to prevent 1 million heart attacks and strokes by 2017.
- Providing resources to states and territories to prevent chronic diseases, including resources to track how well people are taking their blood pressure medicine at the state and county level.
- Reducing cost-sharing through the Affordable Care Act in the Medicare Part D coverage gap and encouraging prescription drug plans to improve medicine use through the Medicare Star Ratings Program. http://go.cms.gov/1VM3k0Z
- Monitoring the health of the nation and setting targets for improvement through the Healthy People 2020 heart disease and stroke objectives. http://go.usa.gov/xjfNw
Health care systems can
- Simplify blood pressure treatment (e.g. prescribe 90-day refills and combination medicines and coordinate pill refills for the same date) and prescribe generic medicines.
- Involve the entire healthcare team at several points of care to ensure patients are taking medicine as directed and to address patient concerns about side effects. Implement effective blood pressure treatment protocols in clinical practice. http://go.usa.gov/xjf59
- Encourage use of home blood pressure monitors and easy-to-use tools (e.g. blood pressure logs and mobile apps) to track and share blood pressure readings.
- Address financial barriers, such as high co-pays and deductibles.
Insurers can
- Incentivize 90-day refills for prescriptions; no or lower co-pays for medicine.
- Use administrative claims data to identify patients who are not taking their medicine correctly and support coordinated care among prescribers, pharmacists, and patients.
- Increase access to Medication Therapy Management services for at-risk patients with chronic disease. http://go.usa.gov/xjfnz
Everyone can
- Follow your healthcare team’s instructions on how much medicine to take, how often, and how long to take it.
- Ask questions about how to correctly take your medicine and why you need them.
- Use a blood pressure monitor at home to keep track of your blood pressure between medical appointments.
- Use weekly pill boxes or a mobile app to keep track of when to take medicine.
- Help loved ones take blood pressure medicine as directed.
Issue Details
Related Pages
- Vital Signs Issue details: Blood Pressure Control, Morbidity and Mortality Weekly Report (MMWR)
- Vital Signs – Blood Pressure Control [PODCAST – 1:15 minutes]
- Vital Signs – Blood Pressure Control [PSA – 0:60 seconds]
- CDC’s Division for Heart Disease and Stroke Prevention
- CDC Heart Disease Website
- CDC Stroke Website
- CDC High Blood Pressure Website
- CDC Interactive atlas of heart disease and stroke
- CDC Evidence Summary: Control High Blood Pressure
Other Sites
- MedlinePlus – Blood Pressure Control
- Centers for Medicare & Medicaid Services
- National Heart, Lung, and Blood Institute
- American Heart Association
Scientific Articles
- Circulation – Medication adherence: its importance in cardiovascular outcomes.
- American Heart Journal – Medication adherence: A call for action.
- Drugs Aging – Medication (re)fill adherence measures derived from pharmacy claims data in older Americans: a review of the literature.
- American Journal of Medicine – Trouble getting started: predictors of primary medication nonadherence.
- Journal of the American College of Cardiology – Poor Adherence to Statin and Antihypertensive Therapies as Risk Factors for Fatal Stroke.
- American Journal of Preventive Medicine – Medication Adherence and Incident Preventable Hospitalizations for Hypertension.
- Medical Care – Association of Antihypertensive Medication Adherence With Healthcare Use and Medicaid Expenditures for Acute Cardiovascular Events.
- Value Health – Impact of interventions on medication adherence and blood pressure control in patients with essential hypertension: a systematic review by the ISPOR medication adherence and persistence special interest group.
- Journal of Behavioral Medicine – Blood pressure outcomes of medication adherence interventions: systematic review and meta-analysis.
- Archives of Internal Medicine – The implications of therapeutic complexity on adherence to cardiovascular medications.
Science Behind the Issue
- Page last reviewed: October 3, 2016
- Page last updated: October 3, 2016
- Content source:
- National Center for Chronic Disease Prevention and Health Promotion
- Page maintained by: Office of the Associate Director for Communications (OADC)


 ShareCompartir
ShareCompartir