Adult Smoking
Focusing on People with Mental Illness
On This Page
February 2013

 1 in 3
1 in 3
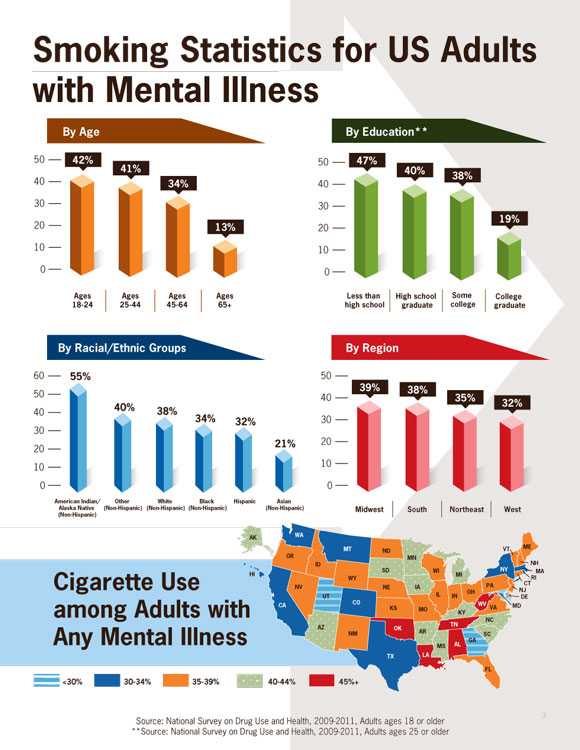
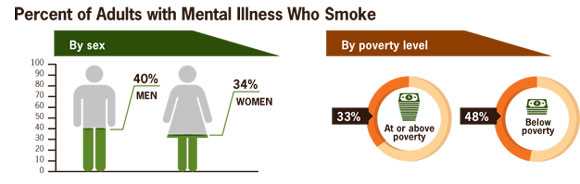
More than 1 in 3 adults (36%) with a mental illness smoke cigarettes, compared with about 1 in 5 adults (21%) with no mental illness.
 3 in 10
3 in 10
About 3 of every 10 cigarettes (31%) smoked by adults are smoked by adults with mental illness.
 1 in 5
1 in 5
Nearly 1 in 5 adults (or 45.7 million adults) have some form of mental illness.*
Cigarette smoking is the leading preventable cause of disease, disability, and death in the US. Despite overall declines in smoking, more people with mental illness smoke than people without mental illness. Because many people with mental illness smoke, many of them will get sick and die early from smoking.
Recent research has shown that, like other smokers, adults with mental illness who smoke want to quit, can quit, and benefit from proven stop-smoking treatments. Some mental health providers and facilities have made progress in this area, while others are now beginning to address tobacco use. The 2006 Surgeon General's Report found that smoke-free policies reduce exposure to secondhand smoke and help smokers quit. Mental health facilities can benefit by making their campuses 100% smoke-free and by making stopping tobacco use part of an overall approach to treatment and wellness. It is critical that people with mental illness get the mental health services they need and are able to get help to quit smoking to improve their overall health and wellness.
*For this report, mental illness is defined as a diagnosable mental, behavioral, or emotional disorder, other than a developmental or substance abuse disorder.
Problem
Smoking is much more common in adults with mental illness than other adults
Smoking and mental illness
- Nicotine has mood-altering effects that put people with mental illness at higher risk for cigarette use and nicotine addiction.
- People with mental illness are more likely to have stressful living conditions, be low income, and lack access to health insurance, health care, and help quitting. All of these factors make it more challenging to quit.
- Evidence shows that there has been direct tobacco marketing to people with mental illness and other vulnerable groups of people.
Smokers who quit have immediate health benefits.
- Risk for a heart attack drops sharply just 1 year after quitting.
- After 2 to 5 years, the chance of stroke can fall to about the same as a nonsmoker's.
- Within 5 years of quitting, the chance of cancer of the mouth, throat, esophagus, and bladder is cut in half.
- Ten years after quitting smoking, the risk for dying from lung cancer drops by half.
Adults with mental illness who smoke want to and are able to quit.
- Like other smokers, smokers with mental illness are interested in quitting, are able to quit, and have a better chance of quitting successfully when they have access to proven stop-smoking treatments.
- With careful monitoring, quitting smoking does not interfere with treatments for mental illness and can be part of the treatment.
- People with mental illness face challenges in quitting smoking and may benefit from extra help to succeed in quitting. This can include more counseling as well as longer use or a combination of stop-smoking medicines.
More attention is needed to help people with mental illness quit smoking.
- Some mental health facilities still allow smoking.
- Some mental health facilities allow smoking as a reward for progress.
- Some mental health facilities now provide counseling and medicine to help smokers quit.
Source: National Survey on Drug Use and Health, 2009-2011, Adults ages 18 or older
Source: National Survey on Drug Use and Health, 2009-2011, Adults ages 18 or older
**Source: National Survey on Drug Use and Health, 2009-2011, Adults ages 25 or older
What Can Be Done
Federal agencies and national partners are working to reduce tobacco use among people with mental illness.
This includes:
- Helping states develop action plans to reduce smoking by people with mental illness.
- Providing funding to promising state and local programs that make stop-smoking treatment part of mental health treatment and wellness.
- Making stop-smoking treatments more available to people who want to quit.
- Conducting research focused on the health and longevity of people with mental illness.
- Providing information to mental health treatment facilities on the benefits of tobacco-free campus policies (i.e., no use of any tobacco product inside the facility or anywhere on its grounds). Several states are already putting these policies in place.
More progress can be achieved:
By mental health professionals
- Asking their patients if they use tobacco; if they do, helping them quit.
- Offering proven quitting treatments, including tailored quit assistance, to patients who use tobacco.
- Referring patients interested in quitting to 1-800-QUIT-NOW, www.smokefree.gov, or other resources.
- Providing more counseling, support, and stop-smoking medicines.
- Making quitting tobacco part of an overall approach to treatment and wellness.
- Monitoring and adjusting mental health medicines as needed in people trying to quit using tobacco.
By mental health facilities
- Including quitting treatments as part of mental health treatment and wellness.
- Stopping practices that encourage tobacco use (such as not providing cigarettes to patients and not allowing staff to smoke with patients).
- Making their entire campus 100% smoke-free as noted in the 2006 Surgeon General’s Report. Several states are already putting these recommendations in place.
By state and community leaders
- Helping mental health and tobacco control programs to work together to reduce tobacco use among people with mental illness.
- Encouraging state mental health and addiction agencies to put in place tobacco quitting programs and tobacco-free campuses.
- Supporting sustained, evidence-based tobacco control programs.
By people with mental illness
- Deciding to quit using tobacco right away. The sooner they stop, the sooner their bodies can begin to heal, and the less likely they are to get sick from tobacco use.
- Asking their doctors and mental health treatment providers for help to quit.
- Calling 1-800-QUIT-NOW for free help quitting and going to www.smokefree.gov for a step-by-step quit guide.
- Avoiding secondhand smoke; making their home and vehicles smoke-free.
- Supporting friends who are trying to quit.
Science Behind the Issue
Related Pages
- Vital Signs issue Details: Current Cigarette Smoking Among Adults Aged ≥ 18 Years with Mental Illness — United States, 2009–2011 Morbidity and Mortality Weekly Report (MMWR)
- CDC’s Smoking & Tobacco Use Web site
- Tips From Former Smokers campaign Web site
- How Tobacco Smoke Causes Disease: What It Means to You
- Secondhand Smoke: What It Means to You
- Vital Signs – Adult Smoking Among People with Mental Illness [PODCAST – 1:16 minutes]
- Adult Smoking Among People with Mental Illness [PSA – 0:60 seconds]
- CDC Feature – Smoking Among Adults With Mental Illness
On Other Web Sites
- The Community Guide: Reducing Tobacco Use and Secondhand Smoke Exposure
- MedlinePlus – Smoking
- MedlinePlus – Quitting Smoking
- MedlinePlus – Mental Disorders
- How to Quit Resources
- Help for Smokers and Other Tobacco Users: Quit Smoking
- SAMHSA (Substance Abuse and Mental Health Services Administration)
- SAMHSA: Smoking & Mental Illness
- SAMHSA: Smoking & Mental Illness [PDF – 578KB]
- Page last reviewed: February 5, 2013
- Page last updated: February 5, 2013
- Content source:
- National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health
- Page maintained by: Office of the Associate Director for Communications (OADC)


 ShareCompartir
ShareCompartir