Chapter 10: Pertussis
Manual for the Surveillance of Vaccine-Preventable Diseases
Printer friendly version [12 pages]
Authors: Amanda Faulkner, MPH; Tami Skoff, MS; Stacey Martin, MSc; Pam Cassiday, MS; Maria Lucia Tondella, PhD; Jennifer Liang, DVM, MPVM
Disease Description
Pertussis, a more commonly known as whooping cough, is a contagious, respiratory disease caused by the bacterium Bordetella pertussis. The illness is characterized by a prolonged paroxysmal cough, which is often accompanied by an inspiratory whoop. Disease presentation varies with age and history of previous exposure or vaccination. Young infants may present to a clinic or hospital with apnea and no other disease symptoms. Adults and adolescents with some immunity may exhibit only mild symptoms or have the typical prolonged paroxysmal cough. In all persons, cough can continue for months.
Pertussis rarely causes severe complications among healthy, vaccinated persons. Infants, however, are at greatest risk for pertussis-related complications and mortality. Pneumonia is the most common complication in all age groups; seizures and encephalopathy generally occur only among very young infants. Death is infrequent and most likely to occur in unvaccinated infants, although fatalities are occasionally reported among older children and adults with serious underlying health conditions.[1]
In addition to B. pertussis, three other Bordetella species can cause disease in humans: B. parapertussis, B. holmesii, and B. bronchiseptica. B. parapertussis cause a pertussis-like illness that is generally milder than pertussis, likely because the bacteria do not produce pertussis toxin. Co-infection of B. pertussis and B. parapertussis is not unusual. Disease attributable to Bordetella species other than B. pertussis is not reportable to CDC.
Background
In the pre-vaccine era, pertussis was a common childhood disease and a major cause of child and infant mortality in the United States. Routine childhood vaccination led to a reduction in disease incidence from an average of 150 reported cases per 100,000 persons between 1922 and 1940, to 0.5 per 100,000 in 1976.[2]The incidence of reported pertussis began increasing in the 1980s, however, and significant peaks in disease have been observed in recent years. In 2012, 48,277 cases were reported nationwide, exceeding levels observed since 1955. Reported pertussis cases decreased during 2013 to 28,639; however, levels remain significantly increased compared to those observed during the 1990s and early 2000s. Multiple factors have likely contributed to the increase including heightened provider and public awareness, improved diagnostic testing, waning immunity from acellular pertussis vaccines, and possibly molecular changes within the pertussis bacterium. The incidence of pertussis remains highest among young infants. In 2013, all pertussis-related deaths (n=13) reported to CDC were among infants less than 6 months of age, who were too young to have received three doses of DTaP vaccine. As of 2013, the second highest incidence of pertussis was observed among school-aged children and adolescents, and the proportion of cases in this age group appears to be increasing.[3-5]
Importance of Rapid Case Identification
Early diagnosis and treatment of pertussis might limit its spread to other susceptible people. When pertussis is strongly suspected, attempts to identify and provide prophylaxis to household and other close contacts at high risk should proceed without waiting for laboratory confirmation. When suspicion of pertussis is low, the investigation can be delayed until there is laboratory confirmation of the diagnosis. However, prophylaxis of pregnant women and infants, as well as their household contacts, should not be delayed.
Importance of Surveillance
Surveillance data collected through case investigations are used to assess impact of disease and monitor changes in epidemiology over time. Surveillance data are also used to guide public health policy and development of control strategies. CDC uses surveillance data to monitor national trends in pertussis and identify populations at risk. Local and state health departments use surveillance data to identify clusters of related cases that might indicate an outbreak.
Laboratory surveillance to monitor changes in the B. pertussis organism is also important. Isolates of B. pertussis collected through routine surveillance have provided researchers with the resources necessary to identify changes in the bacterium, including recent changes in the organism at the molecular level.[6-8] This information is vital to our understanding of the evolution of B. pertussis and how those changes may impact our current pertussis vaccination program and other prevention strategies. See Section VII, “Laboratory Testing” for more details.
Disease Reduction Goals
A disease reduction goal of 2,500 indigenous pertussis cases per year in children <1 year of age, and 2,000 cases per year among adolescents 11 to 18 years of age was proposed as a part of the Healthy People 2020 project.[9] In 2013, 4051 cases were reported among infants less than 1 year of age, while more than 7,000 cases were observed among adolescents 11 to 18 years of age.[5]
Top of PageCase Definitions
The following case definition for pertussis was approved by the Council of State and Territorial Epidemiologists (CSTE) in June 2013 and went into effect January 1, 2014.[10]
Clinical case definition
In the absence of a more likely diagnosis a cough illness lasting ≥ 2 weeks with one of the following symptoms:
- Paroxysms of coughing, OR
- Inspiratory "whoop," OR
- Posttussive vomiting, OR
- Apnea (with or without cyanosis) (FOR INFANTS AGED < 1 YEAR ONLY)
Laboratory criteria for diagnosis
- Isolation of B. pertussis from a clinical specimen
- Positive polymerase chain reaction (PCR) assay for B. pertussis DNA
Epidemiologic Linkage
- Contact with a laboratory-confirmed case of pertussis†*.
Case classification
Probable:
- Meets the clinical case definition, is not laboratory confirmed, and is not epidemiologically linked to a laboratory-confirmed case OR
- FOR INFANTS AGED < 1 YEAR ONLY:
- Acute cough illness of any duration with at least one of the following signs or symptoms:
- Paroxysms of coughing, OR
- Inspiratory "whoop", OR
- Posttussive vomiting, OR
- Apnea (with or without cyanosis)
- Polymerase chain reaction (PCR) positive for pertussis, OR
- Acute cough illness of any duration with at least one of the following signs or symptoms:
- FOR INFANTS AGED < 1 YEAR ONLY:
- Acute cough illness of any duration with at least one of the following signs or symptoms:
- Paroxysms of coughing, OR
- Inspiratory "whoop", OR
- Posttussive vomiting, OR
- Apnea (with or without cyanosis)
- Contact with a laboratory-confirmed case of pertussis
- Acute cough illness of any duration with at least one of the following signs or symptoms:
Confirmed:
- Acute cough illness of any duration with isolation of B. pertussis from a clinical specimen,OR
- Meets the clinical case definition AND is polymerase chain reaction (PCR) positive for pertussis, OR
- Meets the clinical case definition AND had contact with a case laboratory-confirmed case of pertussis
Case Classification Comments:
*Note: An illness meeting the clinical case definition should be classified as “probable” rather than "confirmed" if it occurs in a patient who has contact with an infant aged < 1 year who is polymerase chain reaction (PCR) positive for pertussis and has ≥ 1 sign or symptom and cough duration < 14 days (classified as "probable" case).
†To confirm a case by epidemiologic linkage, the case must be directly linked (i.e., a first-generation contact) to a laboratory-confirmed case by either culture or PCR.[10]
Collection of epidemiologic and clinical data is essential for reporting cases that meet the clinical case definition. Investigators should make every attempt to collect information on paroxysms of cough, whoop, posttussive vomiting, and duration of cough as these variables are required to determine whether an individual meets the clinical case definition for pertussis. When feasible, case investigations initiated shortly after cough onset should include follow-up calls to collect information on cough duration. Follow-up should be done regardless of confirmatory test results so that cases meeting the clinical case definition can be reported. Both probable and confirmed pertussis cases should be reported to the National Notifiable Diseases Surveillance System (NNDSS) by the state health department via the National Electronic Telecommunications System for Surveillance (NETSS) or National Electronic Disease Surveillance System (NEDSS).
Laboratory confirmation of pertussis is important because other pathogens can cause symptoms similar to pertussis. Culture of B. pertussis is the most specific diagnostic test; all patients with cough and a positive B. pertussis culture should be reported as confirmed, even those with cough lasting less than 14 days. PCR is less specific than culture; cases confirmed with only a positive PCR must meet the clinical case definition to be reported as confirmed.
Laboratory Testing
Determining who has pertussis and who does not is often difficult. Whenever possible, a nasopharyngeal swab or aspirate should be obtained from all persons with suspected pertussis. A properly obtained nasopharyngeal swab or aspirate is essential for optimal laboratory diagnosis. Health department personnel and other healthcare practitioners that are asked to obtain these specimens should receive training and supervision from persons experienced in collection of nasopharyngeal specimens. CDC has developed two short training videos for collection of nasopharyngeal aspirate and swab specimens, which can be accessed on the CDC pertussis web site.[21]
Culture
Isolation of B. pertussis by bacterial culture remains the gold standard for diagnosing pertussis. A positive culture for B. pertussis confirms the diagnosis of pertussis. Culture of the organism is also necessary for antimicrobial susceptibility testing and molecular typing.
Although bacterial culture is specific for diagnosis, it is relatively insensitive. Fastidious growth requirements make B. pertussis difficult to isolate. Isolation of the organism using direct plating is most successful during the catarrhal stage (i.e., first 1-2 weeks of cough). Success in isolating the organism declines if the patient has received prior antibiotic therapy effective against B. pertussis, if specimen collection has been delayed beyond the first 2 weeks of illness, and if the patient has been vaccinated.
All persons with suspected cases of pertussis should have a nasopharyngeal aspirate or swab obtained from the posterior nasopharynx for culture. For B. pertussis, nasopharyngeal aspirates will yield similar or higher rates of recovery than nasopharyngeal swabs;[11-14] throat and anterior nasal swabs yield unacceptably low rates of recovery.[15] Therefore, specimens should be obtained from the posterior nasopharynx (Figure 1), not the throat. Specimens should be obtained using polyester, rayon, nylon, or calcium alginate (not cotton) swabs and should be plated directly onto selective culture medium or placed in transport medium. Regan-Lowe agar or freshly prepared Bordet-Gengou medium is generally used for culture; half-strength Regan-Lowe should be used as the transport medium. Specimens should be transported on cold packs and plated at the laboratory within 24 hours.
Polymerase chain reaction for B. pertussis DNA
Polymerase Chain Reaction (PCR) is an important tool for timely diagnosis of pertussis and is increasingly available to clinicians. PCR is a molecular technique used to detect DNA sequences of the Bordetella pertussis bacterium, and unlike culture, does not require viable (live) bacteria present in the specimen.[16, 17]
Despite these advantages, PCR can give results that are falsely-negative or falsely-positive. PCR results can be optimized by avoiding some of the more common pitfalls leading to inaccurate results. Although early signs and symptoms of pertussis are often non-specific, only patients with signs and symptoms consistent with pertussis should be tested. Asymptomatic contacts of confirmed cases should not be tested and testing of contacts should not be used for post-exposure prophylaxis decisions. Falsely-positive results may also occur as a result of specimen contamination, which can occur during specimen collection and testing.[18] The timing of PCR testing for pertussis can significantly affect its ability to accurately diagnose the disease. PCR has optimal sensitivity during the first 3 weeks of cough when bacterial DNA is still present in the nasopharynx. After the fourth week of cough, the amount of bacterial DNA rapidly diminishes, which increases the risk of obtaining falsely-negative results.
Since its inclusion in the case definition in 1997, the proportion of cases confirmed by PCR has increased substantially, and many laboratories now use only PCR to confirm pertussis. However, as of March 2014, there are no standardized PCR assays for pertussis, and assay procedures, as well as sensitivity and specificity, can vary greatly between laboratories. Thus, interpretation criteria for diagnosis vary. Interpretation of PCR results, especially those with high cycle threshold (Ct) values should be done in conjunction with an evaluation of signs and symptoms and available epidemiological information. For more information about interpretation of PCR Ct values, see Best Practices for Health Care Professionals on the use of Polymerase Chain Reaction (PCR) for Diagnosing Pertussis, which is located on the CDC Pertussis Web site.[19]
While PCR is increasingly used as the sole diagnostic test for pertussis, CDC recommends that PCR be used in conjunction with culture when feasible, rather than as an alternative test. Even when a laboratory has validated its PCR method, culturing for B. pertussis should continue; this is especially important to confirm the circulation of B. pertussis when an outbreak is suspected. State laboratories should retain the capability to culture pertussis.
Collection methods for PCR are similar to those for culture, and often the same sample can be used for both tests. However, calcium alginate swabs cannot be used to collect nasopharyngeal specimens for PCR. Swabs used solely for PCR (and not culture) testing may be placed in a sterile tube for transport to the laboratory. Use of liquid transport media is discouraged due to the risk of specimen contamination.
Serologic testing
Commercial serologic tests for pertussis infection can be helpful for diagnosis, especially later in illness. However, there is no commercial kit approved by the FDA for diagnostic use. Cutoff points for diagnostic values of immunoglobulin (Ig) G antibody to pertussis toxin (PT) have not been established, and current IgA and IgM assays lack adequate sensitivity and specificity. In the absence of recent immunization, an elevated serum IgG antibody to PT after 2 weeks of onset of cough is suggestive of recent B. pertussis infection. An increasing titer or a single IgG anti-PT value of approximately 100 IU/mL or greater (using standard reference sera as a comparator) can be used for diagnosis. As of December 2014, positive serology results from commercial laboratories are not confirmatory for the purpose of reporting. A single-point serologic assay has been validated at the Massachusetts state public health laboratory for persons aged 11 years or older and is used for clinical diagnosis and reporting in that state only.[20] A serologic test performed at CDC or at the Massachusetts state laboratory might be used to help investigate outbreaks. In states other than Massachusetts, cases meeting the clinical case definition that are serologically positive but not culture or PCR positive should be reported as probable cases.
Direct fluorescent antibody testing
Direct fluorescent antibody (DFA) testing of nasopharyngeal secretions is sometimes used to screen for pertussis; however, CDC no longer recommends DFA for diagnosing pertussis. Cases meeting the clinical case definition that are DFA positive but not culture or PCR positive should be reported as probable cases.
Pulsed-field gel electrophoresis
Pulsed-field gel electrophoresis (PFGE), a type of DNA fingerprinting, can be performed on B. pertussis isolates to help track transmission (e.g., strains from the same household or small community), but it is not done for routine surveillance.[21, 22]
Inquiries regarding PFGE molecular typing, erythromycin susceptibility testing, serologic testing and other B. pertussis laboratory questions should be directed to the CDC Epidemic Investigations Laboratory: Dr. M. Lucia Tondella, at 404-639-1239, or Ms. Pam Cassiday at 404-639-1231. When sending B. pertussis samples to CDC, please make appropriate arrangements with the laboratory before shipping samples to the address below.
1600 Clifton Road, NE
STAT Unit 12
Atlanta, GA 30333
Additional information on use of the laboratory for support of vaccine-preventable disease surveillance is available in Chapter 22, “Laboratory Support for Surveillance of Vaccine-Preventable Diseases.”
Reporting
Each state and territory has regulations or laws governing the reporting of diseases and conditions of public health importance.[22] These regulations and laws list the diseases to be reported and describe those persons or institutions responsible for reporting, including healthcare providers, hospitals, laboratories, schools, daycare and childcare facilities, and other institutions. Persons reporting should contact the state health department for state-specific reporting requirements.
Reporting to CDC
State health departments should report all probable and confirmed pertussis cases to NNDSS via the NETSS or NEDSS. When provisional information is reported to NNDSS, NETSS and NEDSS reports can be updated as additional information is collected. NETSS and NEDSS accept information about clinical symptoms, laboratory confirmation and vaccination history; this information is included in the Pertussis Surveillance Worksheet (Appendix 11)[2 pages] available for reference and use in case investigation.
Information to collect
Case investigation should include collection of the epidemiologic information listed on the CDC pertussis surveillance worksheet (See Appendix 11[2 pages]). State health departments often supplement the suggested CDC investigation questions with additional information relevant to cases in their communities
Comments on reporting
The limitations of laboratory diagnostics make the clinical case definition essential to pertussis surveillance. It is important to determine duration of cough—specifically, whether it lasts 14 days or longer—in order to determine if a person’s illness meets the definition of a clinical case.
If the first interview is conducted within 14 days of cough onset and cough is still present at the time of interview, it is important to follow up at 14 days or later after onset.
Pertussis case investigation methods vary across state and local health jurisdictions and CDC is committed to helping improve standardization of surveillance practices for pertussis. Please refer to Appendix 11[4 pages] for a detailed instruction sheet describing each data element outlined in the pertussis surveillance worksheet.
Vaccination
The pertussis vaccines currently available in the United States are acellular pertussis antigens in combination with diphtheria and tetanus toxoids (DTaP, DTaP- combination vaccines, and Tdap).
The Advisory Committee on Immunization Practices (ACIP) recommends a four-dose primary series of DTaP, administered at 2, 4, 6 and 15-18 months of age, followed by a fifth booster dose given at 4-6 years.[24] Adolescents and adults should receive a single Tdap booster dose, preferably at ages 11-12 years.[25, 26] Tdap should be administered regardless of time since last tetanus and diphtheria-containing booster.[26] After receipt of Tdap, decennial Td booster doses are recommended. Pregnant women are recommended a dose of Tdap during each pregnancy.[27] To maximize the maternal antibody response and passive antibody transfer to the infant, optimal timing for Tdap administration is between 27 and 36 weeks gestation, although Tdap may be given at any time during pregnancy.[27]
ACIP also recommends:
- Aolescents and adults (e.g., parents, siblings, grandparents, childcare providers, and healthcare personnel) that have or anticipate having close contact with an infant younger than 12 months of age should receive a single dose of Tdap to protect against pertussis if they have not previously received Tdap. Ideally, these persons should receive Tdap at least 2 weeks before beginning close contact with the infant. [28]
- Healthcare personnel should receive a single dose of Tdap as soon as feasible if they have not previously received Tdap and regardless of the time since their most recent Td vaccination. Priority should be given to vaccination of healthcare personnel that have direct contact with infants 12 months of age and younger.[29]
Table 1 lists vaccines likely to appear in case-patients’ vaccination histories. Immunization Information Systems, provider records, and parents are the best sources of this information.
Table 1. Pertussis-containing vaccines.
| Pertussis-Containing Vaccines for Children | Brand | Licensed Date and Used For |
|---|---|---|
| DTaP | INFANRIX DAPTACEL |
First licensed in 1991; used for all childhood doses |
| DTaP+Hib | TriHiBit | Used for the fourth dose only |
| DTap+IPV+HepB | PEDIARIX | Used for the first three doses |
| DTap+IPV+Hib | PENTACEL™ | Approved in 2008; used for primary four-dose series |
| DTap+IPV | KINRIX™ | Approved in 2008; used for booster dose at 4-6 years |
| Pertussis-Containing Vaccines for Adolescents and Adults | Brand | Licensed Date |
| Tdap | ADACEL BOOSTRIX |
First available in 2005 |
| Other Vaccines | Brand | Licensed Date |
| DT/Td | DECAVAC™ TENIVAC™ |
Do not contain pertussis; DT used for primary series when pertussis vaccination was not desired; Td used in persons aged ≥7 years |
Enhancing Surveillance
A number of surveillance activities can improve detection and reporting of cases as well as the completeness and accuracy of the case report form information reported. In addition to those outlined below, Chapter 19, “Enhancing Surveillance,” lists activities that might be applicable to pertussis surveillance.
Assuring appropriate diagnostic testing for pertussis is being performed
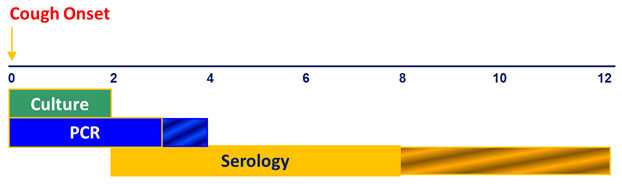
Because no single laboratory test is sufficient for diagnosing pertussis, it is important that available diagnostic tests are used appropriately. To ensure pertussis diagnosis and reporting is optimized, reporting jurisdictions should assess the timing of diagnostic testing relative to cough onset for case-patients identified through routine surveillance. Bacterial culture for pertussis is most useful during the first two weeks of cough and prior to antibiotic use. PCR may effectively diagnose pertussis from 2-4 weeks of cough, and appropriate serologic assays are most useful in the 2-8 weeks following cough onset. Inappropriate diagnostic testing may result in both false-positive and false-negative results, reducing the overall quality of pertussis diagnosis, and ultimately, pertussis surveillance.
Optimal Timing in Weeks for Diagnostic Testing
Unlike many other vaccine-preventable diseases of childhood, pertussis remains endemic in the United States. Cases are expected to occur in all communities; a period of several years in which no cases are reported from a jurisdiction likely reflects failures to diagnose and/or report disease rather than an absence of disease. The level of diagnostic testing being undertaken can be evaluated by reviewing the number of pertussis diagnostic tests (e.g., cultures or PCR results) submitted by a jurisdiction.
Monitoring surveillance indicators
Regular monitoring of surveillance indicators might identify specific areas of the surveillance and reporting system that need improvement. Some suggested surveillance indicators to monitor include:
- Completeness of key data elements collected during pertussis case investigations. Information on clinical presentation, antibiotic treatment, vaccination history, and epidemiologic data are of particular importance and should be collected to the fullest extent possible.
- The proportion of cases reported among infants, children, adolescents, and adults. Jurisdictions with reported pertussis cases heavily weighted toward infants are likely missing a significant proportion of pertussis disease in their community.
- The proportion of cases diagnosed solely with DFA or serologic assays. A high proportion of non-confirmatory laboratory testing for pertussis may be an indication of the need for increased education and promotion of proper pertussis diagnostic testing practices.
- The median interval between onset of cough and notification of state or local public health authorities in probable and confirmed cases.
Expanding Pertussis Data Collection
CDC has partnered with seven states (CO, CT, GA, MN, NM, NY, and OR) participating in the Emerging Infections Program (EIP) Network to conduct enhanced surveillance of pertussis (EPS) and other Bordetella species. EPS is characterized by enhanced case ascertainment and augmented data collection that goes beyond what is requested nationally through NNDSS. Participating sites collect isolates and specimens, when available, for further characterization at the CDC Pertussis and Diphtheria Laboratory. EPS sites also provide the infrastructure for conducting pertussis special studies including those aimed at evaluating pertussis prevention and control strategies.
Other states interested in collecting additional pertussis surveillance information may consider adding the following data elements that are not included currently on the national pertussis surveillance worksheet:
- Cyanosis (Did case-patient experience cyanosis during his/her pertussis infection?)
- Healthcare personnel status (Was case-patient employed as healthcare personnel during his/her pertussis infection?)
- Pregnancy status of female case-patient at cough onset (Was case-patient pregnant or post-partum at time of cough onset?)
- For case-patients <1 year of age:
- Mother’s Tdap vaccination history (Did mother receive Tdap prior to, during, or after her pregnancy with the infant case-patient?)
- Gestational age (in weeks)
Case Investigation
Case investigations generally include reviews of laboratory, hospital, clinic records, and immunization registries, which are the best sources for information about diagnoses and immunization histories. Investigations also include interviews of case-patients, which are necessary to identify sources of infections and contacts at risk. Investigations can include treatment of case-patients and chemoprophylaxis and or vaccination of contacts.
Treatment and chemoprophylaxis
Antimicrobial treatment does not generally lessen the severity of disease unless it is begun in the catarrhal phase, prior to paroxysmal coughing.[25] Treatment reduces transmission and is essential for disease control. The spread of pertussis can be limited by decreasing the infectivity of the patient and by protecting close contacts.[26] Persons with pertussis are infectious from the beginning of the catarrhal stage through the third week after the onset of paroxysms or until 5 days after the start of effective antimicrobial treatment. The recommended antimicrobial agents and doses are the same for treatment and chemoprophylaxis.[27]
Three macrolides are recommended by CDC for treatment of pertussis. Azithromycin is most popular because it is given in a short, simple regimen of one dose each day for 5 days. It is the preferred antimicrobial for use in infants younger than 1 month of age. Similarly, the regimen of two doses a day for 7 days makes clarithromycin another well-accepted choice. Erythromycin, which is given as four doses each day for 14 days, continues to be used, but adherence to the regimen and completion of the course are generally lower than for the other macrolides, and adverse effects (gastrointestinal distress, pyloric stenosis, etc.) occur more frequently. Resistance of B. pertussis to macrolides is rare, and antimicrobial susceptibility testing is not routinely recommended. Testing is appropriate in some circumstances and is recommended when treatment failure is suspected. Refer to Section VII, “Laboratory Testing” for information on how to contact the CDC Pertussis Laboratory to discuss susceptibility testing. If resistance to macrolides is suspected or if their use is contraindicated, CDC recommends treatment with trimethoprim-sulfamethoxazole (TMP-SMZ) in a regimen of two doses a day for 14 days. TMP-SMZ should not be used to treat infants younger than 2 months of age.[27]
CDC recommends administration of chemoprophylaxis to contacts at high risk and household members of a pertussis case-patient. For more specific information on chemoprophylaxis, please see the “Outbreak Control” section of this chapter.
Limited available data suggests Bordetella parapertussis is less susceptible to antibiotics than pertussis; although some studies indicate that erythromycin, azithryomycin, clarithromycin, TMP-SMZ, and ciprofloxacin may have activity against B. parapertussis.[32-39] Because data on the clinical effectiveness of antibiotic treatment are limited, treatment decisions should be based on clinical judgment with particular attention towards special populations, including infants, elderly, and immunocompromised persons; treatment may be warranted to prevent severe outcomes and decrease duration of illness.
Vaccination
During the course of a pertussis investigation, under-vaccinated contacts of pertussis cases may be identified. Contacts younger than 7 years of age who have not received four doses of a pertussis vaccine should complete the series using the minimum recommended catch-up immunization schedule[4 pages].[40] Vaccination with a fifth dose of DTaP is recommended for close contacts aged 4-6 years that have only received four doses. Contacts can be vaccinated with Tdap in accordance with ACIP recommendations. Vaccination is not a substitute for chemoprophylaxis and might not prevent illness in a person who has already been infected with B. pertussis. [24], [30,31], [40,41]
Outbreak Control
Pertussis outbreaks can be difficult to identify and manage. Other respiratory pathogens often cause clinical symptoms similar to pertussis, and co-circulation with other pathogens does occur. To respond appropriately (e.g., provide appropriate prophylaxis), it is important to confirm that B. pertussis is circulating in the outbreak setting and to determine whether other pathogens are contributing to the outbreak. PCR tests vary in specificity, so obtaining culture confirmation of pertussis for at least one suspected case is recommended any time there is suspicion of a pertussis outbreak.
To reduce the risk of pertussis in new mothers and their very young infants, ACIP now recommends that pregnant women receive Tdap vaccine during each pregnancy. During outbreaks, prevention measures should focus on efforts to improve coverage with Tdap during pregnancy to reduce severe illness and possible deaths in vulnerable infants.
With increasing incidence and widespread community transmission of pertussis, extensive contact tracing and broad scale use of postexposure antimicrobial prophylaxis (PEP) among contacts may not be an effective use of limited public health resources. While antibiotics may prevent pertussis disease if given prior to symptom onset, there are no data to indicate that widespread use of PEP among contacts effectively controls or limits the scope of pertussis outbreaks. Another important consideration is the overuse of antibiotics; CDC is engaged in actively promoting the judicious use of antibiotics among healthcare providers and parents.[42] Given these considerations, CDC supports targeting PEP to persons at high risk of developing severe pertussis and to persons who will have close contact with those at high risk of developing severe pertussis.
Accordingly, CDC supports the following:
- Providing PEP to all household contacts of a pertussis case. Within families, secondary attack rates have been demonstrated to be high, even when household contacts are up-to-date with immunizations.[43] Administration of antimicrobial prophylaxis to asymptomatic household contacts within 21 days of onset of cough in the index patient can prevent symptomatic infection.
- Providing PEP to persons within 21 days of exposure to an infectious pertussis case-patient who are at high risk of severe illness. These include:
- Infants and women in their third trimester of pregnancy—severe and sometimes fatal pertussis-related complications occur in infants aged < 12 months, especially among infants < 4 months. Women in their third trimester of pregnancy may be a source of pertussis to their newborn infant.
- All persons with pre-existing health conditions that may be exacerbated by a pertussis infection (for example, but not limited to, immunocompromised persons and patients with moderate to severe medically treated asthma).
- Contacts who themselves have close contact with either infants < 12 months, pregnant women, or individuals with pre-existing health conditions at risk for severe illness or complications.
- All contacts in high risk settings that include infants aged < 12 months or women in the third trimester of pregnancy, which include but are not limited to, neonatal intensive care units, childcare settings, and maternity wards.
- A broader use of PEP in limited closed settings, when the number of identified cases is small, and when a community-wide outbreak is not ongoing; however, when continued transmission of pertussis is evident, multiple rounds of antibiotics would not be recommended. Rather than repeating a course of antibiotics, contacts should be monitored for onset of signs and symptoms of pertussis for 21 days.
Active screening for symptomatic patients with suspected pertussis can be considered during outbreaks in settings such as schools, day care centers, and hospitals. Active screening for suspected cases potentially reduces exposure to persons with pertussis, encourages timely medical evaluation and treatment of cases, and promotes prompt administration of antibiotics to high risk close contacts.[43-50]
References
- Vitek CR, Pascual FB, Baughman AL, Murphy TV. Increase in deaths from pertussis among young infants in the United States in the 1990s. Pediatr Infect Dis J 2003;22:628-34.
- Davis SF, Strebel PM, Cochi SL, Zell ER, Hadler SC. Pertussis surveillance—United States, 1989-1991. MMWR 1992;41(No. SS-8):11-19.
- CDC. Pertussis—United States, 2001-2003. MMWR 2005;54(50):1283-6.
- Guris D, Strebel PM, Bardenheier B, Brennan M, Tachdjian R, Finch E, et al. Changing epidemiology of pertussis in the United States: increasing reported incidence among adolescents and adults, 1990-1996. Clin Infect Dis 1999; 28:1230-7.
- National Notifiable Diseases Surveillance System, 1990-2013. Division of Notifiable Disease Surveillance, Public Health Surveillance Program Office, Office of Surveillance Epidemiology & Laboratory Services, Centers for Disease Control and Prevention, U.S. Department of Health and Human Services, Atlanta, GA 30333.
- Schmidtke AJ, Boney KO, Martin SW, Skoff TH, Tondella ML, Tatti KM. Population diversity among Bordetella pertussis isolates, United States, 1935-2009. Emerg Infect Dis 2012;18:1248-55.
- Pawloski LC, Queenan AM, Cassiday PK, Lynch AS, Harrison M, Shang W, et al. Prevalence and molecular characterization of pertactin-deficient Bordetella pertussis in the US. Clin Vaccin Immunol 2014;21:119-25.
- Martin SW, Pawloski L, Williams M, Weening K, DeBolt C, Qin X, et al. Pertactin-negative B. pertussis strains: evidence for a possible selective advantage. Clin Infect Dis 2014 Oct 9. [Epub ahead of print]
- U.S. Department of Health and Human Services. Office of Disease Prevention and Health Promotion. Healthy people 2020. Washington, DC. Accessed 2014 Dec 12.
- Council of State and Territorial Epidemiologists. CSTE Position Statement 13-ID-15: Revision of the pertussis surveillance case definition to more accurately capture the burden of disease among infants <1 year of age. CSTE, 2013[10 pages].
- Bejuk D, Begovac J, Bace A, Kuzmanovic-Sterk N, Aleraj B. Culture of Bordetella pertussis from three upper respiratory tract specimens. Pediatr Infect Dis J 1995;14:64-5.
- Hallander HO, Reizenstein E, Renemar B, Rasmuson G, Mardin L, Olin P. Comparison of nasopharyngeal aspirates with swabs for culture of Bordetella pertussis. J Clin Microbiol 1993;31:50-2.
- Halperin SA, Bortolussi R, Wort AJ. Evaluation of culture, immunofluorescence, and serology for the diagnosis of pertussis. J Clin Microbiol 1989; 7:752-7.
- Hoppe JE, Weiss A. Recovery of Bordetella pertussis from four kinds of swabs. Eur J Clin Microbiol 1987;6:203-5.
- Loeffelholz M. Bordetella. In: Murray P, Barron E, Jorgenses J, Pfaller M, Yolken R, editors. Manual of clinical microbiology. Washington D.C.: American Society for Microbiology, 2003.
- Koidl C, Bozic M, Burmeister A, Hess M, Marth E, Kessler HH. Detection and differentiation of Bordetella spp. by real-time PCR. J Clin Microbiol 2007;45:347-50.
- Qin X, Galanakis E, Martin ET, Englund JA. Multi-target polymerase chain reaction for diagnosis of pertussis and its clinical implications. J Clin Microbiol 2007;45:506-11.
- Mandal S, Tatti KM, Woods-Stout D, Cassiday PK, Faulkner AE, Griffith MM, et al. Pertussis pseudo-outbreak linked to specimens contaminated by Bordetella pertussis DNA from clinic surfaces. Pediatrics 2012;129:e424-30.
- CDC. Best practices for health care professionals on the use of polymerase chain reaction (PCR) for diagnosing pertussis. 2011. Atlanta, GA: CDC, 2011.
- Marchant CD, Loughlin AM, Lett SM, Todd CW, Wetterlow LH, Bicchieri R, et al. Pertussis in Massachusetts, 1981-1991: incidence, serologic diagnosis, and vaccine effectiveness. J Infect Dis 1994;169:1297-1305.
- Bisgard KM, Christie CD, Reising SF, Sanden GM, Cassiday PK, Gomersall C, et al. Molecular epidemiology of Bordetella pertussis by pulsed-field gel electrophoresis profile: Cincinnati, 1989-1996.J Infect Dis 2001;183:1360-7
- de Moissac YR, Ronald SL, Peppler MS. Use of pulsed-field gel electrophoresis for epidemiological study of Bordetella pertussis in a whooping cough outbreak. J Clin Microbiol 1994;32:398-402.
- CDC. Summary of Notifiable Diseases—United States, 2012. MWWR 2012; 61(53).
- CDC. Pertussis vaccination: Use of acellular pertussis vaccines among infants and young children. Recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR 1997;46(No. RR-7):1-25.
- CDC. Preventing tetanus, diphtheria, and pertussis among adolescents: use of tetanus toxoid, reduced diphtheria toxoid and acellular pertussis vaccines: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR 2006;559(No. RR-3):1-34.
- CDC. Updated recommendations for use of tetanus toxoid, reduced diphtheria toxoid and acellular pertussis (Tdapvaccine from the Advisory Committee on Immunization Practices, 2010. MMWR 2011;60(01):13-15.
- CDC. Updated recommendations for use of tetanus toxoid, reduced diphtheria toxoid, and acellular pertussis vaccine (Tdap) in pregnant women – Advisory Committee on Immunization Practices (ACIP), 2012. MMWR 2013;62(07):131-35.
- CDC. Updated recommendations for use of Tdap in pregnant women and persons who have or anticipate having close contact with an infant aged <12 months – Advisory Committee on Immunization Practices (ACIP), 2011. MMWR 2011;60(41):1424-26.
- CDC. Immunization of health-care personnel – recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR 2011;60(07):1-45.
- CDC. Recommended antimicrobial agents for the treatment and postexposure prophylaxis of pertussis: 2005 CDC Guidelines. MMWR 2005;54(No. RR-14):1–16.
- American Academy of Pediatrics. Pertussis. In: Pickering LK, editor. Red Book: 2003 Report of the Committee on Infectious Diseases. Elk Grove Village, Il: American Academy of Pediatrics 2003: 472-86.
- Mastrantonio P, Stefanelli P, Giuliano M, Herrera Rojas Y, Ciofi degli Atti M, Anemona A, Tozzi AE. Bordetella parapertussis infection in children: epidemiology, clinical symptoms, and molecular characteristics of isolates.J Clin Microbiol 1998;36:999-1002.
- Hoppe JE, Tschirner T. Comparison of media for agar dilution susceptibility testing of Bordetella pertussis and Bordetella parapertussis. Eur J Clin Microbiol Infect Dis 1995;14:775-9.
- Hoppe JE, Bryskier A. In vitro susceptibilities of Bordetella pertussis and Bordetella parapertussis to two ketolides (HMR 3004 and HMR 3647), four macrolides (azithromycin, clarithromycin, erythromycin A, and roxithromycin), and two ansamycins (rifampin and rifapentine). Antimicrob Agents Chemother 1998;42:965-6.
- Hoppe JE, Tschirner T. Comparison of Etest and agar dilution for testing the activity of three macrolides against Bordetella parapertussis. Diagn Microbiol Infect Dis 1997;28:49-51.
- Hoppe JE, Rahimi-Galougahi E, Seibert G. In vitro susceptibilities of Bordetella pertussis and Bordetella parapertussis to four fluoroquinolones (levofloxacin, d-ofloxacin, ofloxacin, and ciprofloxacin), cefpirome, and meropenem. Antimicrob Agents Chemother 1996;40:807-8.
- Hoppe JE, Simon CG. In vitro susceptibilities of Bordetella pertussis and Bordetella parapertussis to seven fluoroquinolones. Antimicrob Agents Chemother 1990;34:2287-8.
- Hoppe JE, Eichhorn A. Activity of new macrolides against Bordetella pertussis and Bordetella parapertussis. Eur J Clin Microbiol Infect Dis 1989;8:653-4.
- Watanabe M, Haraguchi Y. In vitro susceptibility of Bordetella parapertussis to various antimicrobial agents. Antimicrob Agents Chemother1989;33:968-9.
- CDC. Catch-up immunization schedule for persons aged 4 months through 18 years who start late or who are more than 1 month behind — United States, 2014 [4 pages]. (updated 2014 Jan 31; accessed 2014 Dec 14).
- Kurzynski TA, Boehm DM, Rott-Petri JA, Schell RF, Allison PE. Antimicrobial susceptibilities of Bordetella species isolated in a Multicenter Pertussis Surveillance Project.Antimicrob Agents Chemother 1988;32:137-40.
- Centers for Disease Control and Prevention. Get Smart: Know When Antibiotics Work. Atlanta GA [updated: 2013 October 23; accessed 2014].
- Sprauer MA, Cochi SL, Zell ER, Sutter RW, Mullen JR, Englender SJ, Patriarca PA. Prevention of secondary transmission of pertussis in households with early use of erythromycin. Am J Dis Child. 1992;146(2):177-81.
- Dodhia H, Miller E. Review of the evidence for the use of erythromycin in the management of persons exposed to pertussis. Epidemiol Infect 1998;120(2):143-9.
- Halperin SA, Bortolussi R, Langley JM, Eastwood BJ, De Serres G. A randomized, placebo-controlled trial of erythromycin estolate chemoprophylaxis for household contacts of children with culture-positive Bordetella pertussis infection. Pediatrics 1999;104(4):e42
- von König CH. Use of antibiotics in the prevention and treatment of pertussis. Pediatr Infect Dis J 2005;24(5 Suppl):S66-8.
- Alexander EM, Travis S, Booms C, Kaiser A, Fry NK, Harrison TG, Ganpot B, Klein JL. Pertussis outbreak on a neonatal unit: identification of a healthcare worker as the likely source. J Hosp Infect2008;69(2):131-4.
- Elumogo TN, Booth D, Enoch DA, Kuppuswamy A, Tremlett C, Williams CJ, Shankar A, Morter S. Bordetella pertussis in a neonatal intensive care unit: identification of the mother as the likely source. J Hosp Infect2012;82(2):133-5.
- CDC. Recommended antimicrobial agents for the treatment and postexposure prophylaxis of pertussis: 2005 CDC Guidelines. MMWR 2005;54(RR14):1-16. 45.
- Clark TA. Responding to pertussis. J Pediatr2012;161(6):980-2.
- Page last reviewed: May 19, 2015
- Page last updated: May 19, 2015
- Content source:


 ShareCompartir
ShareCompartir