Chlamydia Treatment and Care
Chlamydia is easily cured but can make pregnancy difficult if left untreated.
What is the treatment for chlamydia?
Chlamydia can be easily cured with antibiotics. HIV-positive persons with chlamydia should receive the same treatment as those who are HIV-negative.
Persons with chlamydia should abstain from sexual activity for 7 days after single dose antibiotics or until completion of a 7-day course of antibiotics, to prevent spreading the infection to partners. It is important to take all of the medication prescribed to cure chlamydia. Medication for chlamydia should not be shared with anyone. Although medication will stop the infection, it will not repair any permanent damage done by the disease. If a person’s symptoms continue for more than a few days after receiving treatment, he or she should return to a health care provider to be reevaluated.
Repeat infection with chlamydia is common. Women whose sex partners have not been appropriately treated are at high risk for re-infection. Having multiple chlamydial infections increases a woman's risk of serious reproductive health complications, including pelvic inflammatory disease and ectopic pregnancy. Women and men with chlamydia should be retested about three months after treatment of an initial infection, regardless of whether they believe that their sex partners were successfully treated.
Infants infected with chlamydia may develop ophthalmia neonatorum (conjunctivitis) and/or pneumonia. Chlamydial infection in infants can be treated with antibiotics.
Treatment Guidelines and Updates
- 2015 STD Treatment Guidelines - Chlamydial Infections (June 4, 2015)
Resources for Clinicians
- Chlamydia trachomatis Genital Infection - Journal of Infectious Diseases Supplement, 15 June 2010 (May 21, 2010)
- Clinic-Based Testing for Rectal and Pharyngeal Neisseria gonorrhoeae and Chlamydia trachomatis Infections MMWR July 10, 2009 (July 10, 2009)
- Dear Colleague Letter (July 13, 2009)
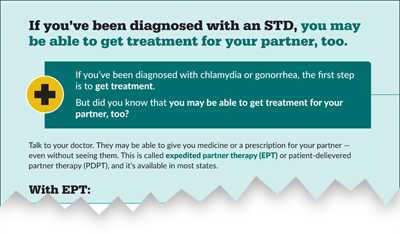
- Expedited Partner Therapy (EPT)
Related Content
- Page last reviewed: December 9, 2016
- Page last updated: March 7, 2017
- Content source:


 ShareCompartir
ShareCompartir