Diagnosis

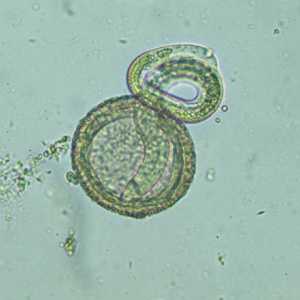
Top: Embryonated egg of B. procyonis, showing the developing larva inside. Bottom: Larva of B. procyonis hatching from an egg. Credit: DPDx
If you suspect you have been infected, consult your health care provider immediately. Be sure to tell your health care provider if you have recently been exposed to raccoons or their feces.
Diagnosis is difficult because symptoms depend on the number of infecting larvae and location in the body. Ocular larva migrans, when the larvae migrate to the eye, can cause sensitivity to light, inflammation of the eye, and blindness. Symptoms of visceral larva migrans, when the larvae travel to organs, depend on which organs are affected. For example, an invasion of the liver may cause hepatomegaly (inflammation and enlargement of the liver), while an invasion of the lung may cause pulmonary symptoms such as cough or chest pain. Larvae rarely end up in the nervous system but the most severe cases are neural larva migrans, when the larvae migrate into the brain and cause it to swell (encephalitis). There is no commercially available test for Baylisascaris infection. A health care provider may test blood, cerebrospinal fluid (CSF), and tissue to determine if an individual is infected. Eye examinations may reveal a migrating larva or lesions and are often the most significant clue to infection with Baylisascaris.
Diagnosis often is made by ruling out other infections that cause similar symptoms. Information on diagnosis and testing can be obtained through your local or state health department or CDC.
More on: Resources for Health Professionals: Diagnosis
Related Materials
- For Lab Staff and Health Care Providers: DPDx: Baylisascariasis
- Page last reviewed: October 11, 2012
- Page last updated: October 11, 2012
- Content source:


 ShareCompartir
ShareCompartir