Evidence-based Laboratory Medicine
Clinical Laboratory Integration into Healthcare Collaborative
(CLIHC™)
Impact on Patient Care
CLIHCTM’s current focus explores the challenges clinicians face for appropriate laboratory test selection and result interpretation. Solutions for these challenges will improve utilization of laboratory services and a reduce diagnostic and treatment errors and delays.
CLIHC™’s Projects
The 2012 CLIHCTM national survey of 1700 internal and family medicine physicians revealed numerous challenges in laboratory service utilization.
Test selection challenges included:
- multiple or confusing test names for the same test
- diverse testing panels with the same name
- differing practice guidelines
- communicating with laboratory professionals
Challenges in result interpretation identified in the survey included:
- variation in laboratory normal values and reporting format
- previous results not readily available
- lack of timely reporting
- results inconsistent with patient’s symptoms
Suggested solutions included:
- CPOE with electronic suggestions for appropriate test ordering
- clinical algorithms/pathways to guide test selection
- interpretive comments
- reflex testing
Communication with laboratory professionals is of particular concern because it was the least frequent among the various ordering and interpretation tactics used in dealing with the challenges. However, when clinicians did consult with laboratory professionals, the majority found it useful. Overuse, underuse, and misuse of laboratory tests may be reduced and patient care improved, if the methods deemed “useful” by the survey respondents can be available to more physicians.
CLIHC™’s projects concentrate on several approaches to support healthcare providers with appropriate laboratory test usage:
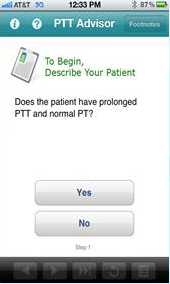
- Development of smartphone/smartpad applications to guide clinicians step-by-step in appropriate coagulation testing
- PTT Advisor app launched in the iTunes store in 2012 guides clinicians in appropriate follow-up testing for patients presenting with a normal prothrombin test (PT) and abnormal partial thromboplastin time (PTT)
- Development of clinical decision support (CDS) mechanisms to help clinicians select the appropriate laboratory test(s) and result interpretation(s) for patient diagnoses. These may include mechanisms such as algorithms, electronic test ordering guidance embedded in the computer physician order entry (CPOE) system or the electronic health record (EHR), and laboratory call centers.
- Survey of US medical schools’ laboratory medicine curriculum
Training, Publications, and Presentations
CLIHC™ training offering continuing education:
Title: Communicating and Collaborating for the Right lab Test and Diagnosis
Description: This podcast is designed to improve the use of laboratory services and facilitate collaborative clinical decision making among primary care physicians and laboratory professionals when selecting the most appropriate laboratory test. Content is derived from a scenario based skit between a clinical pathologist (Mike Laposata, M.D., Ph.D) and internal medicine hospitalist (Jim Meisel, M.D., FACP) that offers insight on the importance of clearly communicating with laboratory professionals to ensure that the most accurate laboratory test is selected in order to obtain an accurate clinical diagnosis for quality patient care.
Objectives:
- Describe at least one diagnostic error related to coagulation testing
- Identify at least two clinical laboratory challenges experienced by clinicians
- List two ways to improve team based care among laboratory professionals and clinicians
To receive continuing education:
- Complete the activity by listening to podcast, available here http://www2c.cdc.gov/podcasts/player.asp?f=8642660
- To receive continuing education, you must complete an evaluation and pass a post-test with a minimum score of 80%: http://www2a.cdc.gov/TCEOnline/registration/detailpage.asp?res_id=5958
Eight peer-reviewed publications from CLIHC™ raised awareness about gaps and potential aids for clinicians’ optimal utilization of clinical laboratory services.
- Oxana Tcherniantchouk, Michael Laposata, and Marisa B. Marques. The isolated prolonged PTT. American Journal of Hematology. 2012; 88 (1): 82-85.
- Passiment E, Meisel J, Fontanesi J, Fritsma G, Aleryani S, Marques M. Decoding laboratory test names: a major challenge to appropriate patient care. J Gen Intern Med. 2013;28(3):453-458.
- Savel TG, Lee BA, Ledbetter G, Brown S, LaValley D, Taylor J, Thompson P. PTT Advisor: A CDC-supported initiative to develop a mobile clinical laboratory decision support application for the iOS platform. J Public Health Informatics. 2013;5(2).
- Hickner J, Thompson P, Wilkinson T, Epner P, Sheehan M, Pollock A, Lee J, Duke C, Jackson B, Taylor J. Primary care physicians’ challenges in ordering clinical laboratory tests and interpreting results. J Am Board Fam Med. 2014;27:268-274.
- Marques M, Hickner J, Thompson P, Taylor J. Primary care physicians and the laboratory. Am J Clin Pathol, 2014;142: 739-740.
- Shirts BH, Jackson BR, Baird GS, Brown JM, Clements B, Grisson R, Hauser RG, Taylor JR, Terrazas E, and Brimhall B. J Pathology Informatics 2015; 6(1): 9.
- Smith B R, Kamoun, M, and Hickner J. Medical Student Education in Laboratory Medicine in United States Medical Schools: A 2014 Status Report. Academic Medicine. 2015; Published ahead of print online.
- Taylor JR, Thompson PJ, Genzen JR, Hickner J, Marques M. Opportunities to Enhance Laboratory Professionals’ Role on the Diagnostic Team. Lab Medicine. 2016: 0: 1-7.
Five Newsletter Reports referenced CLIHC™ work
- Clinical Laboratory News, 2012 – feature story about CLIHC™
- Dark Report, 2012 – highlighted the physician’s survey [PDF 2MB] (http://wwwdev.cdc.gov/ophss/csels/DLS/eblm/pdf/final–the-dark-report-8oct12-p7-8-9.pdf)
- Society to Improve Diagnosis in Medicine, 2013 – highlighted “Decoding laboratory test names” article
- Journal of General Internal Medicine article cited on the Agency for Healthcare Research and Quality (AHRQ), 2013-cited “Decoding laboratory test names” Patient Safety Network(PSNet)
- Clinical Laboratory News, 2014-highlighted the physician’s survey
CLIHC™ presentations given at conferences/meetings:
- Diagnostic Error and the Need for Better Diagnostic Testing” CDC- Medscape Expert Commentary
- Optimizing the Use of Laboratory Testing Services to Improve Patient Diagnosis
- Optimizing Laboratory Test Utilization for Better Patient Care, NLTN Webinar, Julie R. Taylor, April 16, 2014.
- American Society of Clinical Pathology (ASCP) [PDF 2.03MB]
- American Association of Clinical Chemistry (AACC) [PDF 4.3MB]
- COLA [PDF 1.9MB]
- Clinical Laboratory Improvement Advisory Committee (CLIAC) [PDF 264KB]
- Page last reviewed: October 19, 2016
- Page last updated: October 19, 2016
- Content source:


 ShareCompartir
ShareCompartir