STOP STICKS CAMPAIGN

Sharps Injuries
The Centers for Disease Control and Prevention (CDC) estimates that about 385,000 sharps-related injuries occur annually among health care workers in hospitals. More recent data from the Exposure Prevention Information Network (EPINet) suggest these injuries can be reduced, as sharps-related injuries in nonsurgical hospital settings decreased 31.6% during 2001–2006 (following the Needlestick Safety and Prevention Act of 2000). However, injuries in surgical settings increased 6.5% in the same period, where adoption of safety devices was limited compared to nonsurgical settings. It has been estimated about half or more of sharps injuries go unreported. Most reported sharps injuries involve nursing staff, but laboratory staff, physicians, housekeepers, and other health care workers are also injured.

Sharps injuries overview
A sharps injury is a penetrating stab wound from a needle, scalpel, or other sharp object that may result in exposure to blood or other body fluids. Sharps injuries are typically the result of using dangerous equipment in a fast-paced, stressful, and understaffed environment. These strenuous demands often produce feelings of fatigue, frustration, and occasionally anger. In the operating room, for example, health care personnel do not have the luxury of "taking a break," but must continue with their duties until the procedure is completed. These conditions can increase the risk of injury and infection for health care workers.
Health care workers may also incur injuries from improper procedures, such as passing sharps hand-to-hand between team members, placing sharps in a disposal container, or failing to use a safer sharps device. A report from the Exposure Prevention Information Network (EPINet) found that nearly half of all sharps injuries occurred during use of the sharp, and of the nearly 40% of needle injuries which involved a safety designed needle, the majority occurred before activating the safety device. Moreover, the report also showed that many sharps injuries occurred in patient rooms among nurses and operating rooms among surgical team members.1
The cost of a sharps injury can be a compelling reason to use safer sharps practices. One sharps injury can cause a number of direct and indirect costs for the health care facility, including:
- Loss of employee time
- Cost of tying up staff to investigate the injury
- Expense of laboratory testing
- Cost of treatment for infected staff
- Cost of replacing staff
In addition to costs incurred by the health care facility, the stress on the affected worker and the worker’s family can be enormous. In addition to the initial concern, testing for bloodborne pathogens can last for months, producing feelings of anxiety and distress for an extended period of time.
How do sharps injuries occur?
In addition to the use of sharps devices, injuries are also closely associated with certain work practices that can pose an increased risk of bloodborne pathogen exposure. These work practices include:
- Disposal-related activities (11%)
- Activities after use and prior to disposal, such as item disassembly (30%)
- Recapping a used needle (3%)
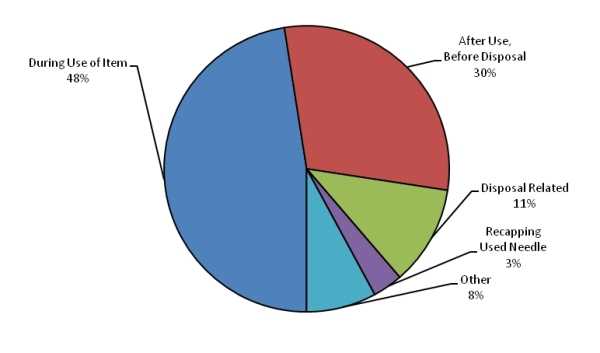
Figure 1: Activities associated with percutaneous injuries in EPINet hospitals, by % total percutaneous injuries (n= 951), 2007 (Source: EPINet [2009]).
What devices are involved with sharps injuries?
Injuries are also closely associated with certain devices that can pose an increased risk of bloodborne pathogen exposure. These devices include:
- Disposable Syringe (31%)
- Suture Needle (24%)
- Winged Steel Needle (5%)
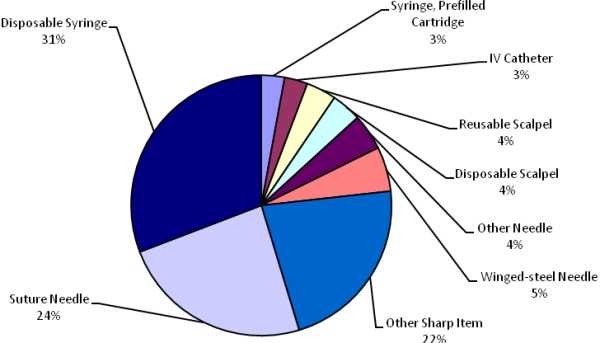
Figure 2: Devices associated with percutaneous injuries in EPINet hospitals, by % total percutaneous injuries (n= 951), 2007 (Source: EPINet [2009]).
1 The EPINet report surveyed 29 health care facilities across the United States, 2007.
- Page last reviewed: June 26, 2013
- Page last updated: June 24, 2011
- Content source:
- Centers for Disease Control and Prevention
- Page maintained by: Office of Associate Director of Communication, Division of Public Affairs


 ShareCompartir
ShareCompartir