Clinical Information
Meningococcal Disease: Technical and Clinical Information
Clinical Features
Fever, headache, and stiff neck in meningococcal meningitis cases, and sepsis and rash in meningococcemia.
Etiologic Agent
There are multiple serogroups of Neisseria meningitidis. Serogroups B, C, and Y cause the majority of disease in the United States and serogroup W causes a small portion of disease. Serogroup A causes disease in developing countries and the meningitis belt of sub-Saharan Africa.
Burden of Disease
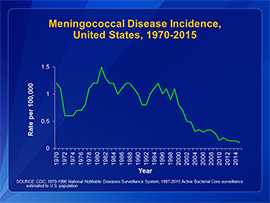
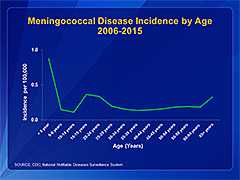
Rates of meningococcal disease have been declining in the United States since the late 1990s (see graph at top right). In 2015, there were about 375 total cases of meningococcal disease reported (incidence rate of 0.18 cases per 100,000 persons). Anyone can get meningococcal disease, but rates of disease are highest in children younger than 1 year, followed by a second peak in adolescence (see graph at bottom right). Among adolescents and young adults, those 16 through 23 years have the highest rates of meningococcal disease.
Sequelae
About 10 to 15 out of 100 people infected with meningococcal disease will die. About 11 to 19 out of every 100 survivors will have long-term disabilities, such as loss of limb(s), deafness, nervous system problems, or brain damage.
Transmission
People spread meningococcal bacteria to others by exchanging respiratory and throat secretions during close or lengthy contact, especially if living in the same household. Humans are the only host. Asymptomatic nasopharyngeal carriers who are not a close contact of a patient with meningococcal disease do not require prophylaxis.
Risk Groups
Household or close contacts of case patients are at the highest risk for developing meningococcal disease. Infants less than one year old and adolescents 16 through 23 years old have higher rates of disease than other age groups. However, cases occur in all age groups including the elderly.
In addition, people with certain medical conditions are at increased risk for meningococcal disease. These medical conditions include
- Functional or anatomic asplenia
- Persistent complement component deficiencies (e.g., C3, C5-9, properdin, factor H, factor D)
- HIV infection
People who take eculizumab (Soliris®), typically for treatment of atypical hemolytic uremic syndrome (aHUS) or paroxysmal nocturnal hemoglobinuria (PNH), are also at increased risk for meningococcal disease. Recent data suggest that meningococcal vaccines likely provide incomplete protection against invasive meningococcal disease in eculizumab patients. Learn more about managing patients who receive eculizumab.
The following groups of people also have an increased risk for meningococcal disease:
- Microbiologists who are routinely exposed to isolates of Neisseria meningitidis
- People identified as being at increased risk because of an outbreak of meningococcal disease
- People traveling to a country where meningococcal disease is epidemic or highly endemic
- First-year college students who live in residence halls
- Military recruits
Learn about CDC’s meningococcal vaccination recommendations, including those for groups at increased risk.
Surveillance
Meningococcal disease is a reportable condition in all states. State and local health departments conduct investigations to ensure all close contacts get prophylaxis. See more about meningococcal disease surveillance.
- Page last reviewed: March 28, 2017
- Page last updated: July 6, 2017
- Content source:
- Content source: National Center for Immunization and Respiratory Diseases



 ShareCompartir
ShareCompartir