Ethiopia: Bringing Laboratory Safety Home
Biosafety cabinets safeguard scientists as they diagnose the world’s most deadly diseases. Ethiopia is reducing its costs and increasing its independence through training a group of engineers to maintain the 120+ biosafety cabinets in Ethiopia’s laboratories.

An engineer in training assessing a biosafety cabinet during a classroom observation period.
As we learned from HIV, Ebola, and other scary microbes, testing a patient’s bodily fluids can be dangerous – even deadly. For laboratory workers who handle these fluids every day, the risk is real and immediate.
In the sub-Saharan country of Ethiopia, health officials have been steadily building a national laboratory system to help detect and control disease outbreaks. Definitive laboratory results are crucial for tracking diseases and getting quick and appropriate care for patients. But to get these results, labs must be able to safely run tests without endangering workers.
Confronting disease threats safely
As Ethiopia’s laboratories become more sophisticated, authorities are placing more emphasis on safety. The workhorse of laboratory safety gear is the biosafety cabinet—an enclosed space that uses a system of airflow and filters to keep workers from breathing in dangerous germs while also preventing the samples inside from becoming contaminated.
This process keeps workers from breathing in dangerous germs and also helps keep the samples inside from becoming contaminated. Getting biosafety cabinets into labs is an important step in being able to diagnose the world’s most deadly diseases.
But simply equipping labs with biosafety cabinets is not enough: the cabinets have to be certified as working properly and maintained and repaired on a regular basis. In Ethiopia, this has meant reliance on foreign experts, who are (a) expensive and (b) not always available when needed.
Increasing independence, decreasing cost

Engineers cleaning the biosafety cabinets in the polio lab.
To address this problem, the Association of Public Health Laboratories, CDC’s National Public Health Institutes program, and the non-profit Eagleson Institute teamed up to offer a multi-course program on how to use, certify, and maintain biosafety cabinets. Eleven engineers took part in the first hands-on training class, held at the Ethiopian Public Health Institute in Addis Ababa over two weeks in February 2016.
According to one participating engineer, Berihu Haile Kahsay, “The biggest benefit of this training is that we are increasing our independence, and the cost will be decreased by having Ethiopian certifiers.”
Investment gets results
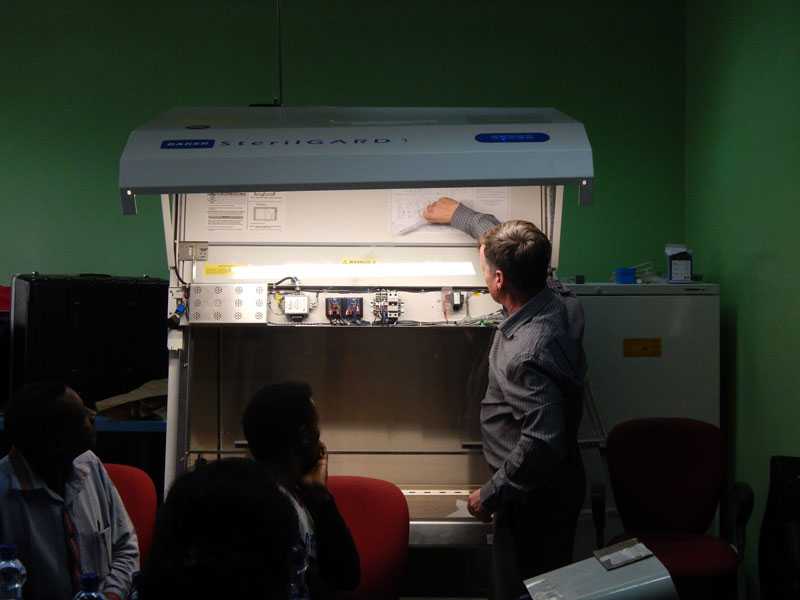
An Eagleson Institute trainer shows how to test in-flow and down-flow on the biosafety cabinets.
The workers are being trained to maintain and repair Class II A2 biosafety cabinets—the type used when testing patient specimens for the microbes that cause HIV, TB, malaria, Hepatitis B, and diarrheal diseases.
Ethiopia’s investment in these and other improvements is paying off: between 2000 and 2012, annual deaths from HIV/AIDS fell from 132 to 55 per 100,000 people. Similarly, between 2000 and 2013, annual TB deaths (among the HIV-negative) fell from 102 to 32 per 100,000 people, and annual malaria deaths fell from 42 to 16 per 100,000 people.
Next Steps
This first group of trained engineers is now testing the 120+ biosafety cabinets in Ethiopia’s laboratories and documenting all problems. Any parts needed to repair the cabinets will be ordered and available in time for the next course in the training program. Eventually, these engineers will be able to repair and certify the biosafety cabinets on their own. And then they can train additional engineers from Ethiopia and other African nations to do the same.
You can’t have an effective public health system without laboratories. And you can’t have effective laboratories without safety systems. Ethiopia is building all three.
About This Story

Engineers fix a light in the biosafety cabinet.
This story illustrates Ethiopia’s commitment to meeting specific targets of the Global Health Security Agenda (GHSA):
- Surveillance: Launch and strengthen global networks for real-time disease surveillance
- Laboratory: A nationwide laboratory system able to safely and accurately detect and characterize pathogens causing epidemic disease
- Biosafety and Biosecurity: Establish an oversight system for pathogen biosafety and biosecurity
Ethiopia is one of 31 countries the U.S. is helping to improve its public health systems through GHSA. The Ethiopian Public Health Institute hosted the training featured in this story in collaboration with the CDC Ethiopia country office. The training is a partnership between the Association of Public Health Laboratories, CDC’s National Public Health Institutes program, and the non-profit Eagleson Institute.
- Page last reviewed: June 27, 2016
- Page last updated: June 27, 2016
- Content source:
Global Health
Notice: Linking to a non-federal site does not constitute an endorsement by HHS, CDC or any of its employees of the sponsors or the information and products presented on the site.


 ShareCompartir
ShareCompartir