Multistate Outbreak of Shiga toxin-producing Escherichia coli O157:H7 Infections Linked to Beef Products Produced by Adams Farm (Final Update)
Posted October 19, 2016 12:15PM EST
This outbreak appears to be over. However, the recalled beef, veal, and bison products may still be in freezers. Consumers who don’t know about the outbreak could continue to eat recalled products and get sick. Read the Recall and Advice to Consumers, Restaurants, and Retailers.
Highlights
- Read the Recall & Advice to Consumers, Restaurants, and Retailers>>
- This outbreak appears to be over. However, the recalled beef, veal, and bison products may still be in freezers. Consumers who don’t know about the outbreak could continue to eat recalled products and may get sick.
- CDC recommends that consumers, restaurants, and retailers do not use, serve, or sell the recalled beef, veal, and bison products.
- These items were shipped to farmers’ markets, retail locations, and restaurants in Massachusetts, Connecticut, and eastern New York. The products also may have been shipped to neighboring states.
- Don’t cook recalled products and eat them. Throw them out or return them to the place of purchase. If you throw them away, put them in a sealed bag in the trash so that children, pets, or other animals can’t eat them.
- Remember to check freezers for recalled products.
- On September 24, 2016, Adams Farm Slaughterhouse recalled beef, veal, and bison products due to possible E. coli O157:H7 contamination. The products, marked with EST. 5497 inside the USDA mark of inspection, include several lot numbers and cuts of meat. The full list can be found on the USDA-FSIS website.
- CDC, several states, and the U.S. Department of Agriculture Food Safety and Inspection Service (USDA-FSIS) investigated this multistate outbreak of Shiga toxin-producing Escherichia coli O157:H7 (STEC O157:H7) infections.
- Eleven people infected with the outbreak strain of STEC O157:H7 were reported from five states.
- Seven ill people were hospitalized. One ill person developed hemolytic uremic syndrome, a type of kidney failure, and no deaths were reported.
- Epidemiologic, traceback, and laboratory evidence indicated that beef products produced by Adams Farm Slaughterhouse in Athol, Massachusetts, were the likely source of this outbreak.
Outbreak Summary
Introduction
CDC collaborated with public health and regulatory officials in several states and the U.S. Department of Agriculture Food Safety and Inspection Service (USDA-FSIS) to investigate a multistate outbreak of Shiga toxin-producing Escherichia coli O157:H7 (STEC O157:H7) infections.
Public health investigators used the PulseNet system to identify illnesses that may be part of this outbreak. PulseNet, coordinated by CDC, is the national subtyping network of public health and food regulatory agency laboratories. PulseNet performs DNA fingerprinting on STEC bacteria isolated from ill people by using techniques called pulsed-field gel electrophoresis (PFGE) and whole genome sequencing (WGS). CDC PulseNet manages a national database of these DNA fingerprints to identify possible outbreaks. In this outbreak, the outbreak strain was defined by PFGE.
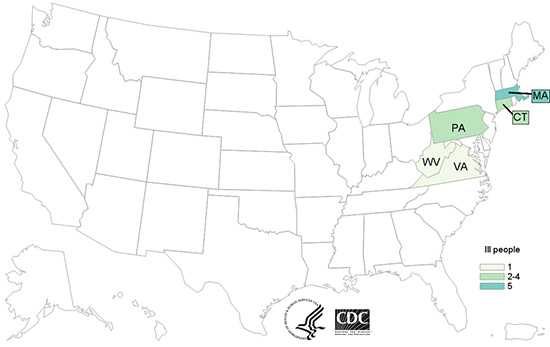
Eleven people infected with the outbreak strain of STEC O157:H7 were reported from five states. A list of the states and the number of cases in each can be found on the Case Count Map page.
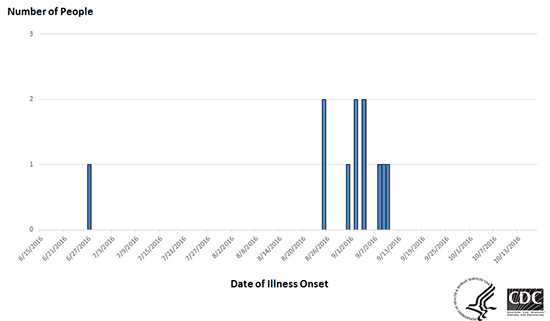
Illnesses started on dates ranging from June 27, 2016 to September 10, 2016. Ill people ranged in age from 1 year to 74, with a median age of 32. Forty-five percent of ill people were female. Seven ill people were hospitalized. One ill person developed hemolytic uremic syndrome, a type of kidney failure, and no deaths were reported.
Investigation of the Outbreak
Epidemiologic, traceback, and laboratory evidence indicated that beef products produced by Adams Farm Slaughterhouse in Athol, Massachusetts, were the likely source of this outbreak.
In interviews, ill people answered questions about the foods they ate and other exposures in the week before they became ill. Seven (100%) of the seven people reached for interview reported eating ground beef in the week before they became ill. Traceback information indicated that six (86%) of these seven ill people ate ground beef produced by Adams Farm Slaughterhouse.
The Connecticut Department of Public Health collected leftover Adams Farm Slaughterhouse ground beef from an ill person’s home and from a restaurant for testing. Test results showed the outbreak strain of STEC O157:H7 in both samples of leftover ground beef.
On September 24, 2016, Adams Farm Slaughterhouse recalled various cuts of beef, veal, and bison products due to possible E. coli O157:H7 contamination. The products originated from animals slaughtered on July 15, 25, and 27, 2016 and August 3, 8, 10, 11, 17, 24, and 26, 2016, and further processed and packed on various dates between July 21 and September 22, 2016. These items were shipped to farmers’ markets, retail locations, and restaurants in Massachusetts, Connecticut, and eastern New York. The products may have been shipped to neighboring states. The products subject to recall have establishment number EST. 5497 inside the USDA mark of inspection and include several lot numbers and cuts of meat. The full list can be found on the USDA-FSIS website.
This outbreak appears to be over. However, the recalled beef, veal, and bison products may still be in freezers. Consumers who don’t know about the outbreak could continue to eat recalled products and get sick. Read the Recall and Advice to Consumers, Restaurants, and Retailers.
October 19, 2016
Final Case Count Update
Since the initial announcement on September 24, four more ill people were reported from Massachusetts (2), Pennsylvania (1), and Virginia (1).
Eleven people infected with the outbreak strain of STEC O157:H7 were reported from five states. A list of the states and the number of cases in each can be found on the Case Count Map page.
Illnesses started on dates ranging from June 27, 2016 to September 10, 2016. Ill people ranged in age from 1 year to 74, with a median age of 32. Forty-five percent of ill people were female. Seven ill people were hospitalized. One ill person developed hemolytic uremic syndrome, a type of kidney failure, and no deaths were reported.
This outbreak appears to be over. However, the recalled beef, veal, and bison products may still be in freezers. Consumers who don’t know about the outbreak could continue to eat recalled products and get sick. Read the Recall and Advice to Consumers, Restaurants, and Retailers.
Initial Announcement
September 24, 2016
CDC is collaborating with public health and regulatory officials in multiple states and the U.S. Department of Agriculture Food Safety and Inspection Service (USDA-FSIS) to investigate a multistate outbreak of Shiga toxin-producing Escherichia coli O157:H7 (STEC O157:H7) infections.
Public health investigators are using the PulseNet system to identify illnesses that may be part of this outbreak. PulseNet, coordinated by CDC, is the national subtyping network of public health and food regulatory agency laboratories. PulseNet performs DNA fingerprinting on STEC bacteria isolated from ill people by using techniques called pulsed-field gel electrophoresis (PFGE) and whole genome sequencing (WGS). CDC PulseNet manages a national database of these DNA fingerprints to identify possible outbreaks. In this outbreak, the outbreak strain was defined by PFGE.
Seven people infected with the outbreak strain of STEC O157:H7 have been reported from four states. A list of the states and the number of cases in each can be found on the Case Count Map page.
Illnesses started on dates ranging from June 27, 2016 to September 4, 2016. Ill people range in age from 1 year to 74, with a median age of 25. Fifty-seven percent of ill people are female. Five ill people have been hospitalized. No one has developed hemolytic uremic syndrome, a type of kidney failure, and no deaths have been reported.
This outbreak can be illustrated with a chart showing the number of people who became ill each day. This chart is called an epidemic curve or epi curve. Illnesses that occurred after September 8, 2016 might not yet be reported due to the time it takes between when a person becomes ill and when the illness is reported. This takes an average of 2 to 3 weeks. Please see the Timeline for Reporting Cases of E. coli O157:H7 Infection for more details.
Investigation of the Outbreak
Epidemiologic, traceback, and laboratory evidence indicate that beef products produced by Adams Farm Slaughterhouse in Athol, Massachusetts is a likely source of this outbreak.
In interviews, ill people answered questions about the foods they ate and other exposures in the week before they became ill. All five (100%) of the five people reached for interview reported eating ground beef in the week before they became ill. Preliminary traceback information indicates that ill people ate ground beef which had been produced by Adams Farm Slaughterhouse.
The Connecticut Department of Public Health collected leftover ground beef from an ill person’s home and from a restaurant for testing; that beef had been produced by Adams Farm Slaughterhouse. Test results showed the outbreak strain ofSTEC O157:H7 in both samples of the leftover ground beef.
On September 24, 2016, Adams Farm Slaughterhouse recalled various cuts of beef, veal, and bison products due to possible E. coli O157:H7 contamination. The products originated from animals slaughtered on July 15, 25, and 27, 2016 and August 3, 8, 10, 11, 17, 24 and 26, 2016, and further processed and packed on various dates between July 21, and September 22, 2016. These items were shipped to farmer’s markets, retail locations, and restaurants in Massachusetts, Connecticut, and eastern New York. The products may have been shipped to neighboring states. The products subject to recall have establishment number EST. 5497 inside the USDA mark of inspection and include several lot numbers and cuts of meat. The full list can be found on the USDA website.
This investigation is ongoing, and we will update the public when more information becomes available. CDC and state and local public health partners are continuing laboratory surveillance through PulseNet to identify additional ill people and to interview those people about foods they ate before they got sick.
More Information

- Page last reviewed: September 24, 2016
- Page last updated: October 19, 2016
- Content Source:


 ShareCompartir
ShareCompartir