Frequently Asked Questions
Prescription opioids are sometimes used to treat moderate-to-severe pain. Because prescription opioids have a number of serious side effects and risks, it is important for you to ask questions, learn more about opioids, and understand their risks. Make sure you’re getting care that is safe, effective, and right for you.
What is the Difference Between Acute Pain and Chronic Pain?
Acute pain usually starts suddenly and has a known cause, like an injury or surgery. It normally gets better as your body heals. Chronic pain is pain lasting 3 months or more and can be caused by a disease or condition, injury, medical treatment, inflammation, or even an unknown reason.
What are Opioids?
Opioids are natural or synthetic chemicals that reduce feelings of pain. Common prescription opioids include:
- Hydrocodone (Vicodin®)
- Oxycodone (OxyContin®)
- Oxymorphone (Opana®)
- Codeine
- Morphine
- Methadone
- Fentanyl
Are Opioids Necessary?
Opioid medications are one of many ways to treat pain. It may be helpful to know that:
- Acute pain: usually starts suddenly and has a known cause, like an injury or surgery. It normally gets better as your body heals.
- Chronic pain: pain lasts 3 months or more and can be caused by a disease or condition, injury, medical treatment, inflammation, or even an unknown reason.
Prescription opioids can be used to treat severe acute pain, but there is no evidence that they are as effective for long-term use. If you’re prescribed an opioid, the best approach is to try the lowest possible dose in the smallest quantity. Opioids should only be used when necessary and only for as long as necessary. Generally, for acute pain this is often 3 days or less; more than 7 days is rarely needed.
Before taking opioid medication for chronic pain:
- Discuss with your doctor pain treatment options, including ones that do not involve prescription drugs.
- Tell your doctor about your medical history and if you or anyone in your family has a history of substance misuse or addiction to drugs or alcohol.
- Discuss all of the risks and benefits of taking prescription opioids.
Talking openly with your healthcare provider will help to make sure you’re getting care that is safe, effective, and right for you. Set up a follow-up appointment with your doctor to reevaluate your pain and, if you have been taking opioids for more than a few days, give you guidance on the best way to cope with possible withdrawal symptoms when you stop.
Will I Get Addicted to Opioids?
Anyone who takes prescription opioids can become addicted to them. You may also develop tolerance—meaning that over time you might need higher doses to relieve your pain, putting you at higher risk for a potentially fatal overdose. You can also develop physical dependence—meaning you have withdrawal symptoms when the medication is stopped.
Tell your doctor about your medical history and if you or anyone in your family has a history of substance misuse or addiction to drugs or alcohol. Also, never take opioids in higher amounts or more often than prescribed.
Can I Avoid Side Effects and Risks?
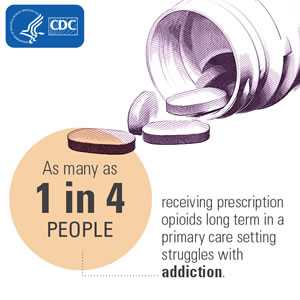
No. Opioids pose a risk to all patients. Anyone taking prescription opioids is at risk for unintentional overdose or death and can become addicted. From 1999 to 2015, more than 183,000 people died from overdose related to prescription opioids in the United States.1 Up to 1 out of 4 people receiving long-term opioid therapy in a primary care setting struggles with opioid use disorder.2,3,4
In addition to the serious risks of opioid use disorder and overdose, the use of prescription opioids can have a number of side effects, even when taken as directed. Review these with your doctor, so you know what you may expect:
- Tolerance—needing to take more of the medication over time for the same pain relief
- Physical dependence—experiencing symptoms of withdrawal when the medication is stopped
- Increased sensitivity to pain
- Constipation
- Nausea and vomiting
- Dry mouth
- Sleepiness and dizziness
- Confusion
- Depression
- Low levels of testosterone that can result in lower sex drive, energy, and strength
- Itching
- Sweating
Remember, your doctor is a partner in your pain treatment plan. It’s important to talk about any and all side effects and concerns to make sure you’re getting the safest and most effective care.
Drug Misuse and Opioid Use Disorder
Opioid Use Disorder (OUD): sometimes referred to as “opioid abuse or dependence,” or “opioid addiction.” OUD is a problematic pattern of opioid use that causes significant impairments at work, school, or home, among other criteria or distress, such as unsuccessful efforts to cut down or control use, social problems, and a failure to fulfill obligations.
What Increases My Risk of Overdose from This Medication?
It is very dangerous to combine opioids with other drugs, especially those that cause drowsiness. Risk of opioid overdose and death increases at higher dosages, and when taken for longer periods of time or more often than prescribed.
Talk to your doctor about any other medications you are using. Work out a plan to call your doctor if you continue to experience pain. Also ask about the serious side effects (like excessive sleepiness or craving more of the medication) so you and your family know when to call a doctor or go to the hospital.
Combinations that Increase Risk
- Alcohol
- Benzodiazepines (also known as “benzos,” including diazepam and alprazolam)
- Other sedatives
- Other opioids (prescription or illicit, including heroin)
What is the Opioid Prescribing Guideline and How Does it Affect Me?
CDC developed the Guideline for Prescribing Opioids for Chronic Pain to help primary care providers make informed prescribing decisions and improve patient care for those who suffer from chronic pain (pain lasting more than 3 months) in outpatient settings. The guideline is not intended for patients who are in active cancer treatment, palliative care, or end-of-life care.
If you have chronic pain and are prescribed opioids as part of your treatment, your doctor should monitor you regularly. This might include extra assessments, a pain treatment plan, more frequent office visits, and urine testing. Prescription opioids can be very dangerous if not used properly. Make sure to follow all of your doctor’s recommendations.
Does CDC Require My Doctor to Follow the Opioid Prescribing Guideline?
No. The Guideline helps providers make informed decisions about pain treatment for patients 18 and older in primary care settings (not active cancer treatment, palliative care, or end-of-life care). The Guideline offers 12 recommendations for opioid prescribing based on research.
Are There Resources to Help Me Learn More about the Risks and Benefits of Opioids?
These web pages will help you learn more about prescription opioids:
References
- CDC. Wide-ranging online data for epidemiologic research (WONDER). Atlanta, GA: CDC, National Center for Health Statistics; 2016. Available at http://wonder.cdc.gov.
- Banta-Green CJ, Merrill JO, Doyle SR, Boudreau DM, Calsyn DA. Opioid use behaviors, mental health and pain—development of a typology of chronic pain patients. Drug Alcohol Depend 2009;104:34–42.
- Boscarino JA, Rukstalis M, Hoffman SN, et al. Risk factors for drug dependence among out-patients on opioid therapy in a large US health-care system. Addiction 2010;105:1776–82.
- Fleming MF, Balousek SL, Klessig CL, Mundt MP, Brown DD. Substance use disorders in a primary care sample receiving daily opioid therapy. J Pain 2007;8:573–82.
- Page last reviewed: October 11, 2017
- Page last updated: October 11, 2017
- Content source:
- Centers for Disease Control and Prevention,
- National Center for Injury Prevention and Control,
- Division of Unintentional Injury Prevention


 ShareCompartir
ShareCompartir