
Tungiasis
[Tunga penetrans]
Causal Agent
The chigoe flea, Tunga penetrans. The flea is also referred to as the jigger, nigua, chica, pico, pique or suthi.
Life Cycle
Eggs are shed by the gravid female into the environment  . Eggs hatch into larvae
. Eggs hatch into larvae  in about 3-4 days and feed on organic debris in the environment. Tunga penetrans has two larval stages before forming pupae
in about 3-4 days and feed on organic debris in the environment. Tunga penetrans has two larval stages before forming pupae  . The pupae are in cocoons that are often covered with debris from the environment (sand, pebbles, etc). The larval and pupal stages take about 3-4 weeks to complete. Afterwards, adults hatch from pupae
. The pupae are in cocoons that are often covered with debris from the environment (sand, pebbles, etc). The larval and pupal stages take about 3-4 weeks to complete. Afterwards, adults hatch from pupae  and seek out a warm-blooded host for blood meals. Both males and females feed intermittently on their host, but only mated females burrow into the skin (epidermis) of the host, where they cause a nodular swelling
and seek out a warm-blooded host for blood meals. Both males and females feed intermittently on their host, but only mated females burrow into the skin (epidermis) of the host, where they cause a nodular swelling  . Females do not have any specialized burrowing organs, and simply claw into the epidermis after attaching with their mouthparts. After penetrating the stratum corneum, they burrow into the stratum granulosum, with only their posterior ends exposed to the environment
. Females do not have any specialized burrowing organs, and simply claw into the epidermis after attaching with their mouthparts. After penetrating the stratum corneum, they burrow into the stratum granulosum, with only their posterior ends exposed to the environment  . The female fleas continue to feed and their abdomens extend up to about 1 cm. Females shed about 100 eggs over a two-week period, after which they die and are sloughed by the host's skin. Secondary bacterial infections are not uncommon with tungiasis.
. The female fleas continue to feed and their abdomens extend up to about 1 cm. Females shed about 100 eggs over a two-week period, after which they die and are sloughed by the host's skin. Secondary bacterial infections are not uncommon with tungiasis.
Geographic Distribution
Tunga penetrans is distributed in tropical and subtropical regions of the world, including Mexico to South America, the West Indies and Africa. The fleas normally occur in sandy climates, including beaches, stables and farms.
Clinical Presentation
The initial burrowing by the gravid females is usually painless; symptoms, including itching and irritation, usually start to develop as the females become fully-developed into the engorged state. Inflammation and ulceration may become severe, and multiple lesions in the feet can lead to difficulty in walking. Secondary bacterial infections, including tetanus and gangrene, are not uncommon with tungiasis.
Tunga penetrans.
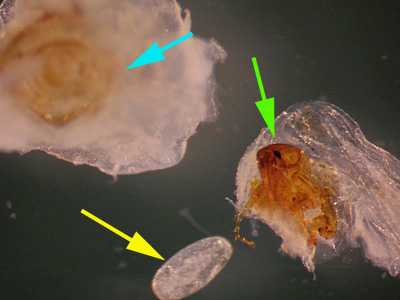
Figure A: Tunga penetrans removed from a lesion on the bottom of the foot of a patient who traveled to Africa. The bulk of the lesion and the posterior part of the flea are marked with a blue arrow. The anterior end of the flea, showing the head, mouthparts and forelegs, is marked with a green arrow. Note the lack of pronotal and genal combs. A single egg (yellow arrow), is also shown.
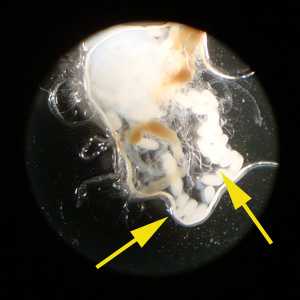
Figure B: Eggs of T. penetrans liberated from the lesion on the second toe of a patient who traveled to Guyana. Image courtesy of Spectrum Health, Grand Rapids, MI.
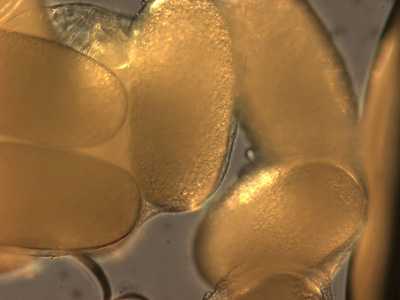
Figure C: Close-up of the eggs from the specimen in Figure B.
Tunga penetrans lesions and biopsy specimens.

Figure A: Gross lesion on a patient's foot caused by T. penetrans. Image courtesy of Drs. Mohammed Asmal and Rocio M. Hurtado. Image first appeared at Partners' Infectious Disease Images (http://www.idimages.orgExternal Web Site Icon), whose content is copyrighted by Partners Healthcare System, Inc., and is used with permission.

Figure B: Gross lesion on a patient's foot caused by T. penetrans. Image courtesy of Drs. Mohammed Asmal and Rocio M. Hurtado. Image first appeared at Partners' Infectious Disease Images (http://www.idimages.orgExternal Web Site Icon), whose content is copyrighted by Partners Healthcare System, Inc., and is used with permission.
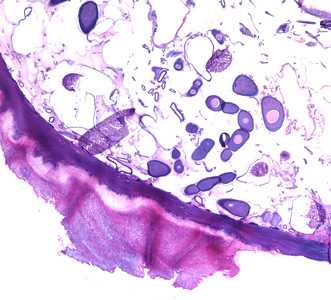
Figure C: Cross-sections of T. penetrans in tissue, stained with hematoxylin and eosin (H&E).
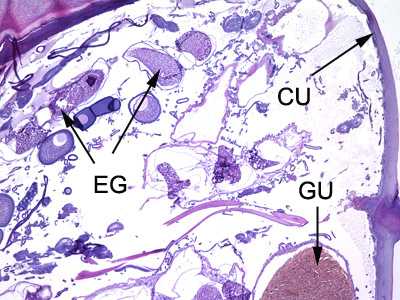
Figure D: Cross-sections of T. penetrans in tissue, stained with hematoxylin and eosin (H&E). In this image, the following structures are labeled: cuticle (CU), gut (GU), and developing eggs (EG).
Laboratory Diagnosis
Identification is made by the finding of adult fleas and their eggs in lesions.
Treatment Information
Treatment is usually limited to extraction of the whole flea from the skin using a sterile needle. Care should be taken not to burst the flea, which can lead to severe inflammation. No available drug has yet been demonstrated to be effective in treating tungiasis. Patients with evidence of superinfection should be treated topically with a broad-spectrum antibiotic. Antibiotic treatment should be systemic if the superinfection is severe. Tetanus prophylaxis is indicated for patients whose tetanus vaccination status is unknown or not up-to-date.
DPDx is an education resource designed for health professionals and laboratory scientists. For an overview including prevention and control visit www.cdc.gov/parasites/.
- Page last reviewed: May 3, 2016
- Page last updated: May 3, 2016
- Content source:
- Global Health – Division of Parasitic Diseases and Malaria
- Notice: Linking to a non-federal site does not constitute an endorsement by HHS, CDC or any of its employees of the sponsors or the information and products presented on the site.
- Maintained By:


 ShareCompartir
ShareCompartir