
Trichomoniasis
[Trichomonas vaginalis]
Causal Agent
Trichomonas vaginalis, a flagellate, is the most common pathogenic protozoan of humans in industrialized countries.
Life Cycle
Trichomonas vaginalis resides in the female lower genital tract and the male urethra and prostate  , where it replicates by binary fission
, where it replicates by binary fission  . The parasite does not appear to have a cyst form, and does not survive well in the external environment. Trichomonas vaginalis is transmitted among humans, its only known host, primarily by sexual intercourse
. The parasite does not appear to have a cyst form, and does not survive well in the external environment. Trichomonas vaginalis is transmitted among humans, its only known host, primarily by sexual intercourse  .
.
Geographic Distribution
Worldwide. Higher prevalence among persons with multiple sexual partners or other venereal diseases.
Clinical Presentation
Trichomonas vaginalis infection in women is frequently symptomatic. Vaginitis with a purulent discharge is the prominent symptom, and can be accompanied by vulvar and cervical lesions, abdominal pain, dysuria and dyspareunia. The incubation period is 5 to 28 days. In men, the infection is frequently asymptomatic; occasionally, urethritis, epididymitis, and prostatitis can occur.
Trichomonas vaginalis trophozoites.
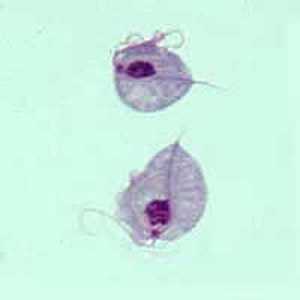
Figure A: Two trophozoites of T. vaginalis obtained from in vitro culture, stained with Giemsa.

Figure B: Trophozoite of T. vaginalis in a vaginal smear, stained with Giemsa.
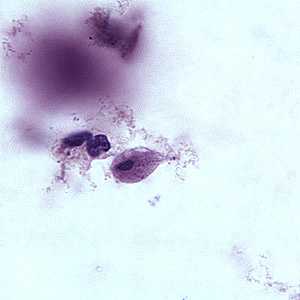
Figure C: Trophozoite of T. vaginalis in a vaginal smear, stained with Giemsa.
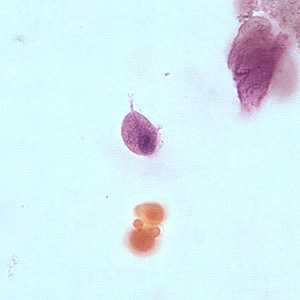
Figure D: Trophozoite of T. vaginalis in a vaginal smear, stained with Giemsa.
Laboratory Diagnosis
Microscopic examination of wet mounts may establish the diagnosis by detecting actively motile organisms. This is the most practical and rapid method of diagnosis (allowing immediate treatment), but it is relatively insensitive. Direct immunofluorescent antibody staining is more sensitive than wet mounts, but technically more complex. Culture of the parasite is the most sensitive method, but results are not available for 3 to 7 days. In women, examination should be performed on vaginal and urethral secretions. In men, anterior urethral or prostatic secretions should be examined.
Treatment Information
Trichomoniasis can be cured with a single dose of prescription antibiotic medication (either metronidazole or tinidazole), pills which can be taken by mouth. It is okay for pregnant women to take this medication. Some people who drink alcohol within 24 hours after taking this kind of antibiotic can have uncomfortable side effects.
People who have been treated for trichomoniasis can get it again. About 1 in 5 people get infected again within 3 months after treatment. To avoid getting reinfected, make sure that all of your sex partners get treated too, and wait to have sex again until all of your symptoms go away (about a week). Get checked again if your symptoms come back.
DPDx is an education resource designed for health professionals and laboratory scientists. For an overview including prevention and control visit www.cdc.gov/parasites/.
- Page last reviewed: May 3, 2016
- Page last updated: May 3, 2016
- Content source:
- Global Health – Division of Parasitic Diseases and Malaria
- Notice: Linking to a non-federal site does not constitute an endorsement by HHS, CDC or any of its employees of the sponsors or the information and products presented on the site.
- Maintained By:


 ShareCompartir
ShareCompartir