
Sparganosis
[Spirometra mansoni] [Spirometra ranarum] [Spirometra mansonoides] [Spirometra erinacei] ['Sparganum proliferum']
Causal Agents
Cestodes in the genus Spirometra, including S. mansoni, S. ranarum, S. mansonoides and S. erinacei, as well as the aberrant Sparganum proliferum.
Life Cycle
Adult members of the genus Spirometra live in the intestines of dogs and cats  . Eggs are shed in feces
. Eggs are shed in feces  and embryonate in the environment
and embryonate in the environment  . Eggs hatch in water and release coracidia
. Eggs hatch in water and release coracidia  , which are ingested by copepods. The coracidia develop into procercoid larvae in the copepod intermediate host
, which are ingested by copepods. The coracidia develop into procercoid larvae in the copepod intermediate host  . Second intermediate hosts, including fish, reptiles and amphibians, ingest infected copepods and acquire procercoid larvae. The procercoid larvae develop into plerocercoid larvae in the second intermediate host
. Second intermediate hosts, including fish, reptiles and amphibians, ingest infected copepods and acquire procercoid larvae. The procercoid larvae develop into plerocercoid larvae in the second intermediate host  . The cycle is completed when a predator (dog or cat) eats an infected second intermediate host
. The cycle is completed when a predator (dog or cat) eats an infected second intermediate host  . Humans cannot serve as definitive hosts for Spirometra spp., but serve as paratenic or second intermediate hosts
. Humans cannot serve as definitive hosts for Spirometra spp., but serve as paratenic or second intermediate hosts  and develop sparganosis. Humans acquire sparganosis by either drinking water contaminated with infected copepods or consuming the flesh of an under-cooked second intermediate or paratenic host. Spargana can live up to 20 years in the human host.
and develop sparganosis. Humans acquire sparganosis by either drinking water contaminated with infected copepods or consuming the flesh of an under-cooked second intermediate or paratenic host. Spargana can live up to 20 years in the human host.
Geographic Distribution
The genus Spirometra occurs worldwide in distribution, although most human cases of sparganosis are recorded from southeast Asian countries. Sparganosis is endemic in animals throughout North America, although human cases from this area are rare.
Clinical Presentation
Migrating spargana cause various symptoms depending on the final location in the host. Spargana may locate anywhere, including subcutaneous tissue, breast, orbit, urinary tract, pleural cavity, lungs, abdominal viscera and the central nervous system. The migration in subcutaneous tissues is usually painless, but when spargana settle in the brain or spine a variety of neurological symptoms may occur, including weakness, headache, seizure, and abnormal skin sensations, such as numbness or tingling. If the inner ear is involved, the patient may experience vertigo or deafness. Occasionally, Sparganum proliferum can cause proliferative lesions in the infected tissue, with multiple plerocercoids present in a single site.
Proliferating spargana in groin tissue.
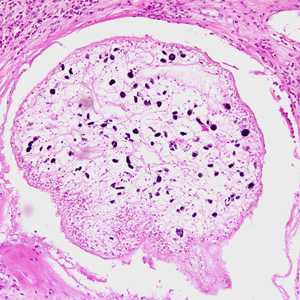
Figure A: Proliferating sparganum in groin tissue of a patient from Paraguay, stained with hematoxylin and eosin (H&E).
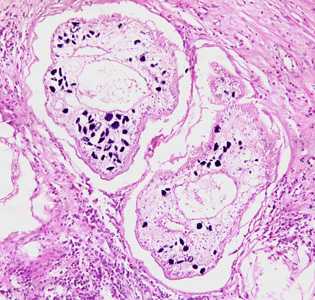
Figure B: Proliferating spargana in groin tissue of a patient from Paraguay, stained with hematoxylin and eosin (H&E).
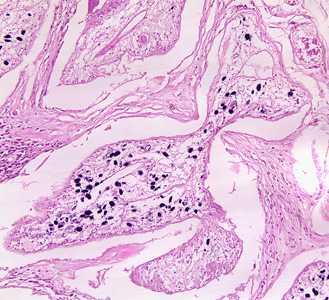
Figure C: Proliferating sparganum in groin tissue of a patient from Paraguay, stained with hematoxylin and eosin (H&E).
Proliferating spargana in lung tissue.
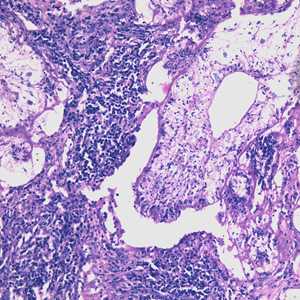
Figure A: Proliferating sparganum in lung tissue in a patient from Taiwan, stained with hematoxylin and eosin (H&E).
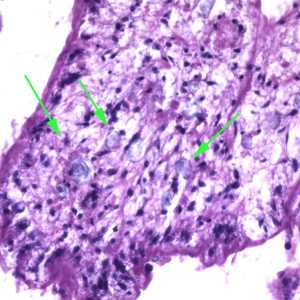
Figure B: Higher magnification of the sparganum in Figure A. In this image, calcareous corpuscles (green arrows) can be seen.
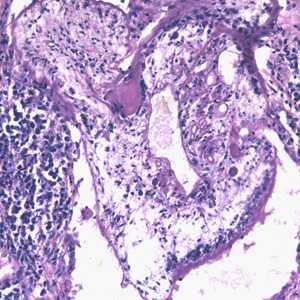
Figure C: Proliferating sparganum in lung tissue in a patient from Taiwan, stained with H&E.
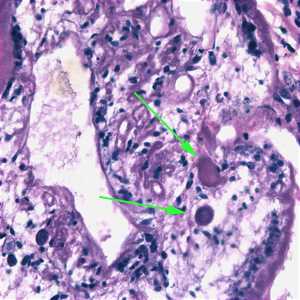
Figure D: Higher magnification of the sparganum in Figure C. In this image, calcareous corpuscles (green arrows) can be seen.
Spargana removed from tissue
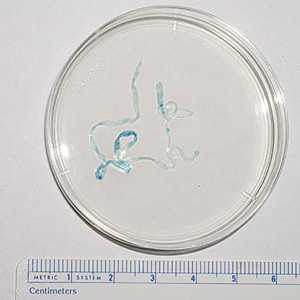
Figure A: Sparganum removed from the chest wall of a patient. The worm measured about 70 mm long. Images from a specimen courtesy of the Oklahoma State Department of Health.
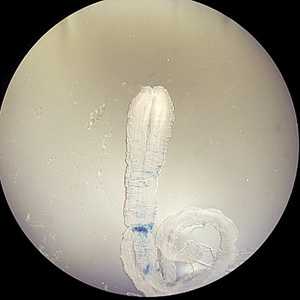
Figure B: Sparganum removed from the chest wall of a patient. The worm measured about 70 mm long. Images from a specimen courtesy of the Oklahoma State Department of Health.
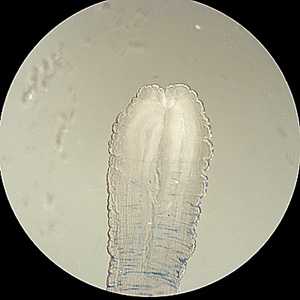
Figure C: Close-up of the anterior end of the sparganum in Figures A and B. Note the end is thickened and wrinkled, and possesses a characteristic cleft-like invagination.

Figure D: Sparganum removed from the ocular conjunctiva of a patient from Taiwan. The worm measured 40 mm long. Image courtesy of Dr. John H. Cross and the Uniformed Services University of the Health Sciences, Bethesda, MD.
Laboratory Diagnosis
Diagnosis is usually made by the recovery of a sparganum from infected tissue. The presence of a sparganum is diagnostic and identification to the species level is usually not warranted. However, the best way to identify the species is to infect an appropriate definitive host with a living sparganum and identify the adult after maturation.
Treatment Information
Surgical removal is the treatment of choice for sparganosis. Generally, treatment with mebendazole, albendazole, or praziquantel is not effective to treat infection with these larvae. In rare cases of proliferative sparganosis, prolonged treatment with mebendazole and praziquantel have been used in addition to surgical removal with mixed success.
DPDx is an education resource designed for health professionals and laboratory scientists. For an overview including prevention and control visit www.cdc.gov/parasites/.
- Page last reviewed: May 3, 2016
- Page last updated: May 3, 2016
- Content source:
- Global Health – Division of Parasitic Diseases and Malaria
- Notice: Linking to a non-federal site does not constitute an endorsement by HHS, CDC or any of its employees of the sponsors or the information and products presented on the site.
- Maintained By:


 ShareCompartir
ShareCompartir