
Pthiriasis
[Pthirus pubis]
Causal Agent
Pthirus pubis, the pubic or crab louse, is an insect of the order Psocodea and is an ectoparasite whose only host are humans.
Life Cycle
Pubic lice (Pthirus pubis) have three stages: egg, nymph and adult. Eggs (nits) are laid on a hair shaft  . Females will lay approximately 30 eggs during their 3-4 week life span. Eggs hatch after about a week and become nymphs, which look like smaller versions of the adults. The nymphs undergo three molts (
. Females will lay approximately 30 eggs during their 3-4 week life span. Eggs hatch after about a week and become nymphs, which look like smaller versions of the adults. The nymphs undergo three molts ( ,
,  ,
,  ) before becoming adults
) before becoming adults  . Adults are 1.5-2.0 mm long and flattened. They are much broader in comparison to head and body lice. Adults are found only on the human host and require human blood to survive. If adults are forced off the host, they will die within 24-48 hours without a blood feeding. Pubic lice are transmitted from person to person most-commonly via sexual contact, although fomites (bedding, clothing) may play a minor role in their transmission.
. Adults are 1.5-2.0 mm long and flattened. They are much broader in comparison to head and body lice. Adults are found only on the human host and require human blood to survive. If adults are forced off the host, they will die within 24-48 hours without a blood feeding. Pubic lice are transmitted from person to person most-commonly via sexual contact, although fomites (bedding, clothing) may play a minor role in their transmission.
Geographic Distribution
Pthiriais is common and is distributed worldwide.
Clinical Presentation
The majority of infestations are asymptomatic. When symptoms are noted they may include a tickling feeling of something moving in the hair, itching, caused by the an allergic reaction to louse saliva, and irritability. Pruritis caused by the bites of pubic lice may be very intense, and discoloration of the skin may occur if the infestation is left untreated for an extended length of time.
Modes of Transmission:
The main mode of transmission is person to person by sexual contact with someone who is already infested. Fomites (bedding, clothing) may play a minor role, although rare.
Pthirus pubis, adults and nymphs.
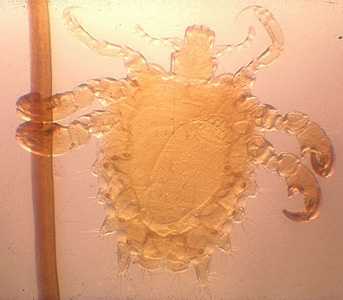
Figure A: Adult female P. pubis. An egg can be seen within her body cavity.

Figure B: Adult male of P. pubis.
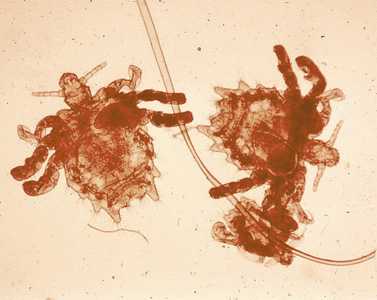
Figure C: Three specimens of P. pubis on a hair shaft.

Figure D: Nymph of P. pubis.
Pthirus pubis, eggs (nits).
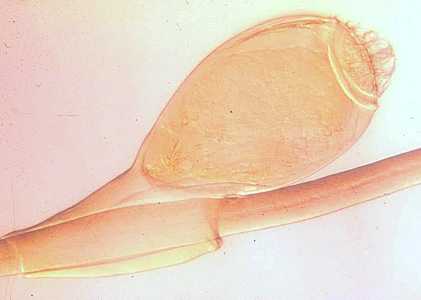
Figure A: Egg (nit) of P. pubis.
Diagnostic Findings
The diagnosis of pthiriasis is best made by finding a live nymph, adult louse, or a nit on the hair of a person, usually in the pubic or perianal area, although they may also be found on armpit, moustache and chest hairs.
Treatment Information
- Both over-the-counter and prescription medications are available for treatment of pubic lice infestations.
- A lice-killing lotion containing 1% permethrin or a mousse containing pyrethrins and piperonyl butoxide can be used to treat pubic ("crab") lice. These products are available over-the-counter without a prescription at a local drug store or pharmacy. These medications are safe and effective when used exactly according to the instructions in the package or on the label.
- Lindane shampoo is a prescription medication that can kill lice and lice eggs. However, lindane is not recommended as a first-line therapy. Lindane can be toxic to the brain and other parts of the nervous system; its use should be restricted to patients who have failed treatment with or cannot tolerate other medications that pose less risk. Lindane should not be used to treat premature infants, persons with a seizure disorder, women who are pregnant or breast-feeding, persons who have very irritated skin or sores where the lindane will be applied, infants, children, the elderly, and persons who weigh less than 110 pounds.
- Malathion* lotion 0.5% (Ovide*) is a prescription medication that can kill lice and some lice eggs; however, malathion lotion (Ovide*) currently has not been approved by the U.S. Food and Drug Administration (FDA) for treatment of pubic ("crab") lice.
- Oral ivermectin has been used successfully to treat lice; however, ivermectin currently has not been approved by the U.S. Food and Drug Administration (FDA) for treatment of lice.
How to treat pubic lice infestations: (Warning: See special instructions for treatment of lice and nits on eyebrows or eyelashes. The lice medications described in this section should not be used near the eyes.)
- Wash the infested area; towel dry.
- Carefully follow the instructions in the package or on the label. Thoroughly saturate the pubic hair and other infested areas with lice medication. Leave medication on hair for the time recommended in the instructions. After waiting the recommended time, remove the medication by following carefully the instructions on the label or in the box.
- Following treatment, most nits will still be attached to hair shafts. Nits may be removed with fingernails or by using a fine-toothed comb.
- Put on clean underwear and clothing after treatment.
- To kill any lice or nits remaining on clothing, towels, or bedding, machine-wash and machine-dry those items that the infested person used during the 2–3 days before treatment. Use hot water (at least 130°F) and the hot dryer cycle.
- Items that cannot be laundered can be dry-cleaned or stored in a sealed plastic bag for 2 weeks.
- All sex partners from within the previous month should be informed that they are at risk for infestation and should be treated.
- Persons should avoid sexual contact with their sex partner(s) until both they and their partners have been successfully treated and reevaluated to rule out persistent infestation.
- Repeat treatment in 9–10 days if live lice are still found.
- Persons with pubic lice should be evaluated for other sexually transmitted diseases (STDs).
Special instructions for treatment of lice and nits found on eyebrows or eyelashes:
- If only a few live lice and nits are present, it may be possible to remove these with fingernails or a nit comb.
- If additional treatment is needed for lice or nits on the eyelashes, careful application of ophthalmic-grade petrolatum ointment (only available by prescription) to the eyelid margins 2–4 times a day for 10 days is effective. Regular Vaseline* should not be used because it can irritate the eyes if applied.
* Use of trade names is for identification only and does not imply endorsement by the Public Health Service or by the U.S. Department of Health and Human Services.
DPDx is an education resource designed for health professionals and laboratory scientists. For an overview including prevention and control visit www.cdc.gov/parasites/.
- Page last reviewed: May 3, 2016
- Page last updated: May 3, 2016
- Content source:
- Global Health – Division of Parasitic Diseases and Malaria
- Notice: Linking to a non-federal site does not constitute an endorsement by HHS, CDC or any of its employees of the sponsors or the information and products presented on the site.
- Maintained By:


 ShareCompartir
ShareCompartir