
Paragonimiasis
[Paragonimus westermani] [Paragonimus spp.]
Causal Agents
More than 30 species of trematodes (flukes) of the genus Paragonimus have been reported which infect animals and humans. Among the more than 10 species reported to infect humans, the most common is P. westermani, the oriental lung fluke.
Life Cycle
The eggs are excreted unembryonated in the sputum, or alternately they are swallowed and passed with stool . In the external environment, the eggs become embryonated
. In the external environment, the eggs become embryonated , and miracidia hatch and seek the first intermediate host, a snail, and penetrate its soft tissues
, and miracidia hatch and seek the first intermediate host, a snail, and penetrate its soft tissues . Miracidia go through several developmental stages inside the snail
. Miracidia go through several developmental stages inside the snail : sporocysts
: sporocysts , rediae
, rediae , with the latter giving rise to many cercariae
, with the latter giving rise to many cercariae , which emerge from the snail. The cercariae invade the second intermediate host, a crustacean such as a crab or crayfish, where they encyst and become metacercariae. This is the infective stage for the mammalian host
, which emerge from the snail. The cercariae invade the second intermediate host, a crustacean such as a crab or crayfish, where they encyst and become metacercariae. This is the infective stage for the mammalian host . Human infection with P. westermani occurs by eating inadequately cooked or pickled crab or crayfish that harbor metacercariae of the parasite
. Human infection with P. westermani occurs by eating inadequately cooked or pickled crab or crayfish that harbor metacercariae of the parasite . The metacercariae excyst in the duodenum
. The metacercariae excyst in the duodenum , penetrate through the intestinal wall into the peritoneal cavity, then through the abdominal wall and diaphragm into the lungs, where they become encapsulated and develop into adults
, penetrate through the intestinal wall into the peritoneal cavity, then through the abdominal wall and diaphragm into the lungs, where they become encapsulated and develop into adults . (7.5 to 12 mm by 4 to 6 mm). The worms can also reach other organs and tissues, such as the brain and striated muscles, respectively. However, when this takes place completion of the life cycles is not achieved, because the eggs laid cannot exit these sites. Time from infection to oviposition is 65 to 90 days. Infections may persist for 20 years in humans. Animals such as pigs, dogs, and a variety of feline species can also harbor P. westermani.
. (7.5 to 12 mm by 4 to 6 mm). The worms can also reach other organs and tissues, such as the brain and striated muscles, respectively. However, when this takes place completion of the life cycles is not achieved, because the eggs laid cannot exit these sites. Time from infection to oviposition is 65 to 90 days. Infections may persist for 20 years in humans. Animals such as pigs, dogs, and a variety of feline species can also harbor P. westermani.
Geographic Distribution
Paragonimus spp. are distributed throughout the Americas, Africa and southeast Asia. Paragonimus westermani is distributed in southeast Asia and Japan. Paragonimus kellicotti is endemic to North America.
Clinical Presentation
The acute phase (invasion and migration) may be marked by diarrhea, abdominal pain, fever, cough, urticaria, hepatosplenomegaly, pulmonary abnormalities, and eosinophilia. During the chronic phase, pulmonary manifestations include cough, expectoration of discolored sputum, hemoptysis, and chest radiographic abnormalities. Extrapulmonary locations of the adult worms result in more severe manifestations, especially when the brain is involved.
Eggs of Paragonimus spp. in unstained wet mounts.

Figure A: Egg of P. westermani in an unstained wet mount.

Figure B: Egg of P. westermani in an unstained wet mount.
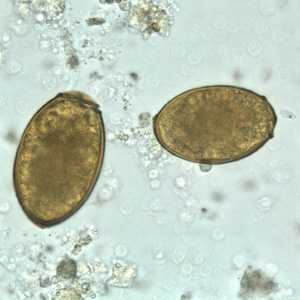
Figure C: Eggs of P. westermani in an unstained wet mount.

Figure D: Egg of P. westermani in an unstained wet mount.
Eggs of Paragonimus spp. in tissue.
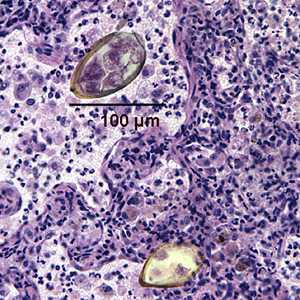
Figure A: Eggs of Paragonimus sp. taken from a lung biopsy stained with hematoxylin and eosin (H&E). These eggs measured 80-90 µm by 40-45 µm. The species was not identified in this case.
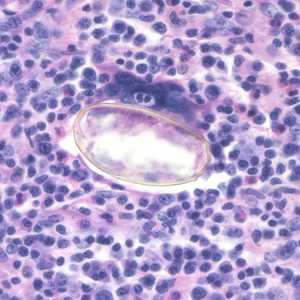
Figure B: Egg of Paragonimus sp. taken from a lung biopsy stained with hematoxylin and eosin (H&E). This egg measured 80-90 µm by 40-45 µm. The species was not identified in this case.
Eggs of Paragonimus kellicotti.
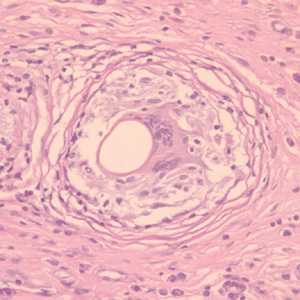
Figure A: Cross-section of an egg of P. kellicotti in a lung biopsy specimen, stained with periodic acid-Schiff (PAS) stain. Image courtesy of Dr. Gary Procop.
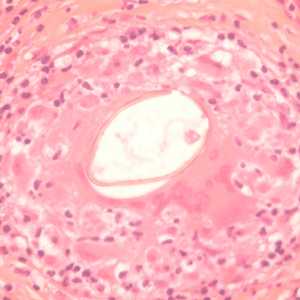
Figure B: Longitudinal section of an egg of P. kellicotti in a lung biopsy specimen, stained with hematoxylin and eosin (H&E). Image courtesy of Dr. Gary Procop.
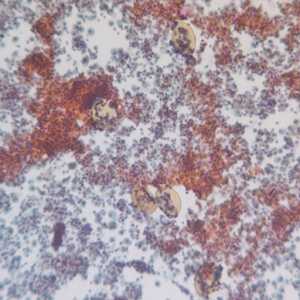
Figure C: Egg of P. kellicotti in a Pap-stained bronchial alveolar lavage (BAL) specimen at 100x magnification. Image courtesy of Dr. Gary Procop.
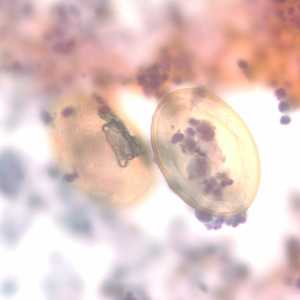
Figure D: Eggs of P. kellicotti in a Pap-stained bronchial alveolar lavage (BAL) specimen at 400x magnification. Image courtesy of Dr. Gary Procop.
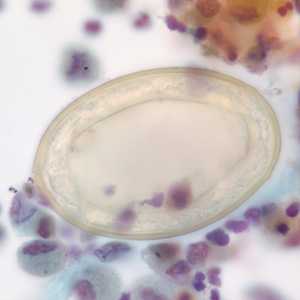
Figure E: Higher magnification (1000x, oil) of the specimen in Figures C and D. Image courtesy of Dr. Gary Procop.
Adults of Paragonimus spp.

Figure A: Adult of P. westermani.
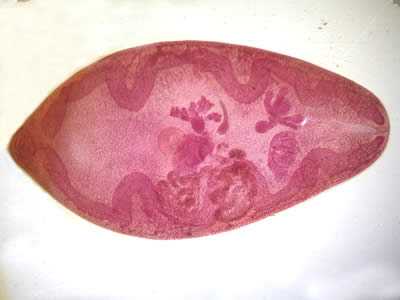
Figure B: Higher magnification of the adult fluke seen in Figure A.

Figure C: Adult of Paragonimus sp., taken from a lung biopsy specimen stained with hematoxylin and eosin (H&E). Note the presence of the oral sucker. The species was not identified in this case.
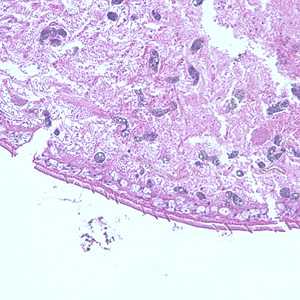
Figure D: Higher magnification of Figure C, showing a close-up of the cuticle.
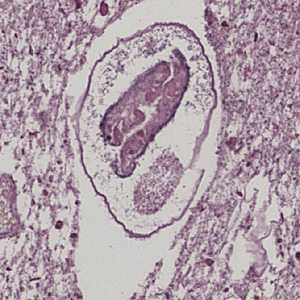
Figure E: Adult of P. kellicotti taken from a lung biopsy specimen stained with H&E. This worm is in poor condition, indicating it was probably an old infection. Image courtesy of Dr. Miguel Madariaga, University of Nebraska Medical Center.
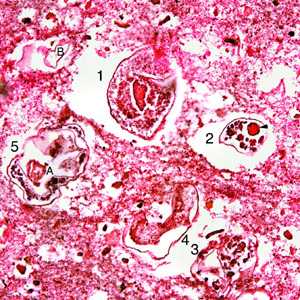
Figure F: Sections of several adults of P. kellicotti taken from a pleural biopsy stained with H&E. Numbers 1-5 show the individual worms. The integument is gone from most of the worms, as this was probably an old infection, but remnants of the gonad (A, dart) and uterine tubes (B) can be seen. Image courtesy of Dr. Miguel Madariaga, University of Nebraska Medical Center. Image first appeared in: Madariaga, MD, M. G., T. Ruma, MD, and J. H. Theis, MD. 2007. Autochthonous human paragonimiasis in North America. Wilderness & Environmental Medicine. 18(3): 203-205. Image used with permission of © Allen Press Publishing Services.
Laboratory Diagnosis
Morphologic Diagnosis
Diagnosis is based on microscopic demonstration of eggs in stool or sputum, but these are not present until 2 to 3 months after infection. (Eggs are also occasionally encountered in effusion fluid or biopsy material.) Concentration techniques may be necessary in patients with light infections. Biopsy may allow diagnostic confirmation and species identification when an adult or developing fluke is recovered.
More on: Morphologic comparison with other intestinal parasites.
Antibody Detection
Pulmonary paragonimiasis is the most common presentation of patients infected with Paragonimus spp., although extrapulmonary (cerebral, abdominal) paragonimiasis may occur. Detection of eggs in sputum or feces of patients with paragonimiasis is often very difficult; therefore, serodiagnosis may be very helpful in confirming infections and for monitoring the results of individual chemotherapy. In the United States, detection of antibodies to Paragonimus westermani has helped physicians differentiate paragonimiasis from tuberculosis in Indochinese immigrants. The complement fixation (CF) test has been the standard test for paragonimiasis; it is highly sensitive for diagnosis and for assessing cure after therapy. Because of the technical difficulties of CF, enzyme immunoassay (EIA) tests were developed as a replacement. The immunoblot (IB) assay performed with a crude antigen extract of P. westermani has been in use at CDC since 1988. Positive reactions, based on demonstration of an 8-kDa antigen-antibody band were obtained with serum samples of 96% of patients with parasitologically confirmed P. westermani infection. Specificity was >99%; of 210 serum specimens from patients with other parasitic and non-parasitic infections, only 1 serum sample from a patient with Schistosoma haematobium reacted. Antibody levels detected by EIA and IB do decline after chemotherapeutic cure but not as rapidly as those detected by the CF test. Most published literature deals with pulmonary paragonimiasis due to P. westermani although in some geographic areas other Paragonimus species cause similar or distinct clinical manifestations in human infections. Cross-reactivity between species does occur but at varying levels for different species. Thus, use of a test for P. westermani may not allow detection of antibodies to other Paragonimus species.
Reference:
Slemenda SB, Maddison SE, Jong EC, Moore DD. Diagnosis of paragonimiasis by immunoblot. Am J Trop Med Hyg 1988;39:469-471.Treatment Information
Praziquantel is the drug of choice: adult or pediatric dosage, 25 mg/kg given orally three times per day for 2 consecutive days.
Alternative: Triclabendazole, adult or pediatric dosage, 10 mg/kg orally once or twice. For cerebral disease, a short course of corticosteroids may be given with the praziquantel to help reduce the inflammatory response around dying flukes.
Triclabendazole is not commercially available in the United States, it is not approved by the Food and Drug Administration. However, it is available through CDC, under an investigational protocol.
Praziquantel
Oral praziquantel is available for human use in the United States.
Note on Treatment in Pregnancy
DPDx is an education resource designed for health professionals and laboratory scientists. For an overview including prevention and control visit www.cdc.gov/parasites/.
- Page last reviewed: May 3, 2016
- Page last updated: May 3, 2016
- Content source:
- Global Health – Division of Parasitic Diseases and Malaria
- Notice: Linking to a non-federal site does not constitute an endorsement by HHS, CDC or any of its employees of the sponsors or the information and products presented on the site.
- Maintained By:


 ShareCompartir
ShareCompartir