
Case #223 - March, 2008
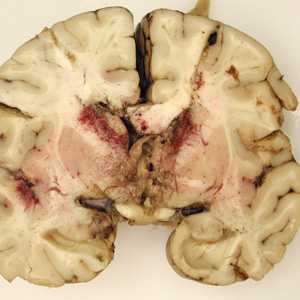
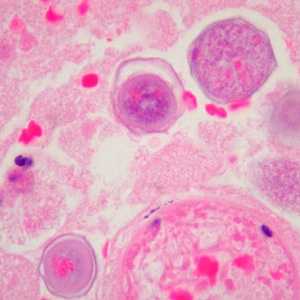
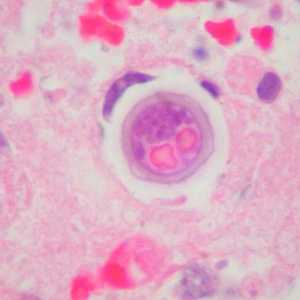
A seven-year-old, previously healthy child developed flu-like symptoms and rapidly progressive bulbar palsy, coma, and eventually death. Imaging revealed florid ventriculitis. A viral etiology was initially suspected. The autopsy revealed extensive necrotizing (mixed inflammatory, occasional giant cells, vasculitic) granulomatous encephalitis (Figures A and B), with a subependymal necroinflammatory process. Tissue sections of the brain were made and stained with hematoxylin and eosin (H&E). Images of the brain and subsequent tissue sections (Figures C and D, taken at 1000x oil magnification) were sent to DPDx for diagnostic assistance. What is your diagnosis? Based on what criteria? What further testing is recommended?

Case Answer
This was a case of granulomatous amebic encephalitis (GAE) caused by Balamuthia mandrillaris. Diagnostic features were:
- the pathology of the infection, manifesting as rapid granulomatous encephalitis.
- the presence of thick-walled cysts (Figures C and D), containing a fibrous outer wall (ectocyst) and an inner wall (endocyst) with granular cytoplasm and prominent globules.
Balamuthia is one of four genera of typically free-living amoebae implicated in amebic encephalitis, the other three being Naegleria, Acanthamoeba, and only recently, Sappinia. Amoebae enter the body through nasal passages or broken skin and can invade the central nervous system by hematogenous dissemination. Identification to the genus level is sometimes difficult based on morphology of the amoebae alone. In this particular case, Naegleria could have been ruled-out by the presence of cysts, as this genus does not produce cysts in human tissue. This case was confirmed by an immunofluorescence test and real-time PCR using Balamuthia-specific primers. Cultivation of the causal organism may also prove useful.
More on: Free-living Amoebae
The case and the images were kindly contributed by Dr. Carlos Galliani and the Cook Children’s Hospital in Fort Worth, TX.
Images presented in the monthly case studies are from specimens submitted for diagnosis or archiving. On rare occasions, clinical histories given may be partly fictitious.
DPDx is an education resource designed for health professionals and laboratory scientists. For an overview including prevention and control visit www.cdc.gov/parasites/.
- Page last reviewed: August 24, 2016
- Page last updated: August 24, 2016
- Content source:
- Global Health – Division of Parasitic Diseases and Malaria
- Notice: Linking to a non-federal site does not constitute an endorsement by HHS, CDC or any of its employees of the sponsors or the information and products presented on the site.
- Maintained By:


 ShareCompartir
ShareCompartir