
Case #200 - March, 2007
Approximately one and a half months after a trip to Costa Rica, a man developed a papule on the back of his right hand. The papule progressed to a 2 cm ulcer with a raised border. The ulcer was not tender but was draining serous fluid, and the surrounding skin was red and swollen. A second, similar eruption occurred on the same hand, and the man sought medical attention. His physician gathered clinical and travel history, examined the lesions, and contacted the Division of Parasitic Diseases for assistance. Tissue scrapings and a punch biopsy were collected. Suspicious objects were reported by the pathologists who reviewed the slides. Specimens were sent to DPD’s reference diagnostic laboratory for review. Figures A-C, taken at 1000× magnification, show what was seen on a Giemsa stained smear of a tissue scraping. What is your diagnosis? Based on what criteria? What other testing, if any, is indicated?
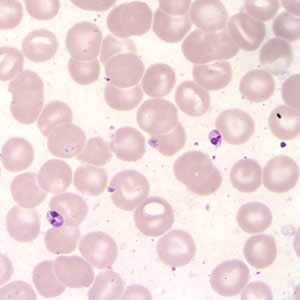
Figure A

Figure B
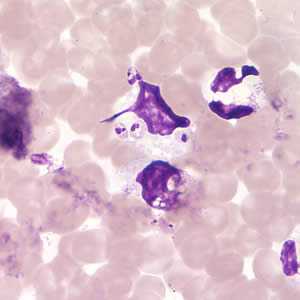
Figure C
Case Answer
This was a case of New World Cutaneous Leishmaniasis caused by Leishmania sp. In the Americas, several species within the two subgenera Leishmania and Viannia are potential causative agents. Diagnostic features included the presence of amastigotes, some within macrophages. Amastigotes are the small (1-5 µm in length), oval-shaped structures with a prominent nucleus and rod-shaped kinetoplast. Size was not given in the case scenario, although it can be extrapolated from the average size of a red blood cell.
Some amastigotes may appear rounded and the kinetoplast may not be visible. It is imperative to observe both a nucleus and a kinetoplast in order to make accurate identification of an amastigote. Since all species of Leishmania are practically indistinguishable morphologically, tissue specimens and aspirates can be useful for culture and PCR. In this case, isoenzyme analysis indicated that the causal agent was Leishmania (Viannia) panamensis.
The Division of Parasitic Diseases’ reference diagnostic laboratory uses several testing techniques, and requests multiple specimens per technique, to increase sensitivity. Slide examination (to observe amastigotes) and culture (to observe promastigotes) are performed. Additional testing such as PCR and serology can be added to the diagnostic algorithm, if circumstances warrant and material is available. Serology is of limited use in cases of cutaneous leishmaniasis.
More on: Leishmaniasis
Images presented in the monthly case studies are from specimens submitted for diagnosis or archiving. On rare occasions, clinical histories given may be partly fictitious.
DPDx is an education resource designed for health professionals and laboratory scientists. For an overview including prevention and control visit www.cdc.gov/parasites/.
- Page last reviewed: August 24, 2016
- Page last updated: August 24, 2016
- Content source:
- Global Health – Division of Parasitic Diseases and Malaria
- Notice: Linking to a non-federal site does not constitute an endorsement by HHS, CDC or any of its employees of the sponsors or the information and products presented on the site.
- Maintained By:


 ShareCompartir
ShareCompartir