
Giardiasis
[Giardia duodenalis (syn. G. lamblia, G. intestinalis)]
Causal Agents
Giardia duodenalis is a protozoan flagellate (Diplomonadida).
Life Cycle:
Cysts are resistant forms and are responsible for transmission of giardiasis. Both cysts and trophozoites can be found in the feces (diagnostic stages)  . The cysts are hardy and can survive several months in cold water. Infection occurs by the ingestion of cysts in contaminated water, food, or by the fecal-oral route (hands or fomites)
. The cysts are hardy and can survive several months in cold water. Infection occurs by the ingestion of cysts in contaminated water, food, or by the fecal-oral route (hands or fomites)  . In the small intestine, excystation releases trophozoites (each cyst produces two trophozoites)
. In the small intestine, excystation releases trophozoites (each cyst produces two trophozoites)  . Trophozoites multiply by longitudinal binary fission, remaining in the lumen of the proximal small bowel where they can be free or attached to the mucosa by a ventral sucking disk
. Trophozoites multiply by longitudinal binary fission, remaining in the lumen of the proximal small bowel where they can be free or attached to the mucosa by a ventral sucking disk  . Encystation occurs as the parasites transit toward the colon. The cyst is the stage found most commonly in nondiarrheal feces
. Encystation occurs as the parasites transit toward the colon. The cyst is the stage found most commonly in nondiarrheal feces  . Because the cysts are infectious when passed in the stool or shortly afterward, person-to-person transmission is possible. While animals are infected with Giardia, their importance as a reservoir is unclear.
. Because the cysts are infectious when passed in the stool or shortly afterward, person-to-person transmission is possible. While animals are infected with Giardia, their importance as a reservoir is unclear.
Geographic Distribution:
Worldwide, more prevalent in warm climates, and in children.
Clinical Presentation
The spectrum varies from asymptomatic carriage to severe diarrhea and malabsorption. Acute giardiasis develops after an incubation period of 1 to 14 days (average of 7 days) and usually lasts 1 to 3 weeks. Symptoms include diarrhea, abdominal pain, bloating, nausea, and vomiting. In chronic giardiasis the symptoms are recurrent and malabsorption and debilitation may occur.
Giardia duodenalis cysts in wet mounts stained with iodine.

Figure A: G. duodenalis cyst in a wet mount stained with iodine.
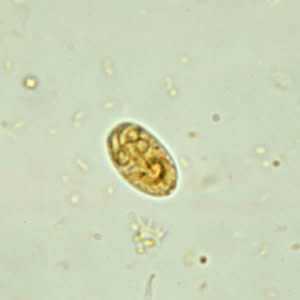
Figure B: G. duodenalis cyst in a wet mount stained with iodine.

Figure C: G. duodenalis cyst in a wet mount stained with iodine.

Figure D: G. duodenalis cyst in a wet mount stained with iodine.

Figure E: G. duodenalis cyst in a wet mount stained with iodine.

Figure F: G. duodenalis cyst in a wet mount stained with iodine.
Giardia duodenalis cysts in wet mounts under differential interference contrast (DIC) microscopy.
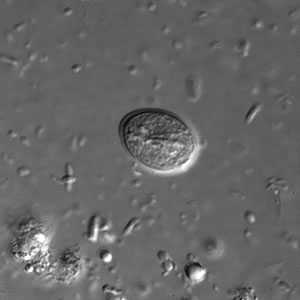
Figure A: G. duodenalis cyst in a wet mount under differential interference contrast (DIC) microscopy. Image taken at 1000× magnification.

Figure B: Two G. duodenalis cysts in a wet mount under DIC microscopy; image taken at 1000× magnification.
G. duodenalis cysts in trichrome stain.
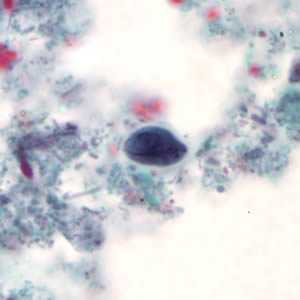
Figure A: G. duodenalis cyst stained with trichrome.
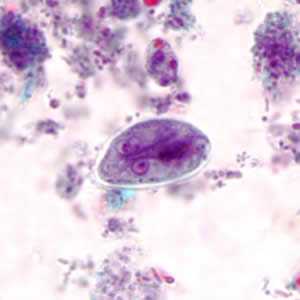
Figure B: G. duodenalis cyst stained with trichrome.
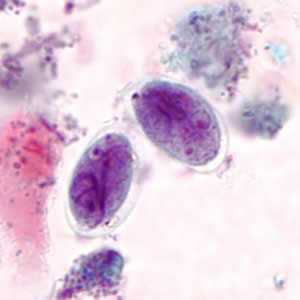
Figure C: G. duodenalis cysts stained with trichrome.
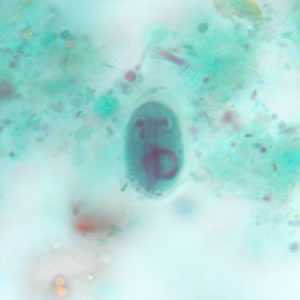
Figure D: G. duodenalis cyst stained with trichrome.
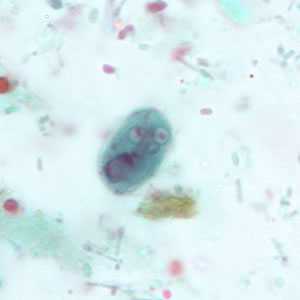
Figure E: G. duodenalis cyst stained with trichrome.
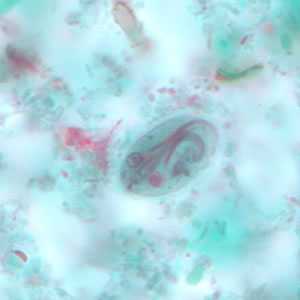
Figure F: G. duodenalis cyst stained with trichrome.
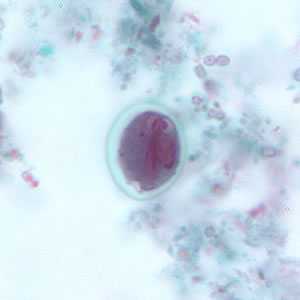
Figure G: G. duodenalis cyst stained with trichrome. Sometimes the cytoplasm of the cyst may retract from the cell wall.
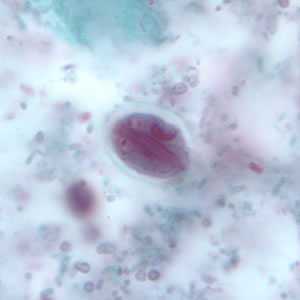
Figure H: G. duodenalis cyst stained with trichrome. Sometimes the cytoplasm of the cyst may retract from the cell wall.
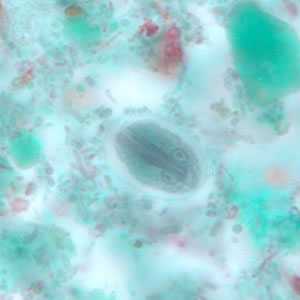
Figure I: G. duodenalis cyst stained with trichrome. Sometimes the cytoplasm of the cyst may retract from the cell wall.
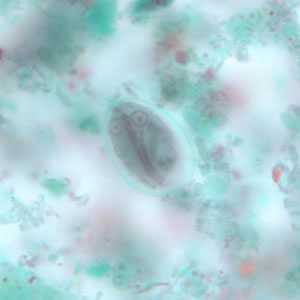
Figure J: G. duodenalis cyst stained with trichrome. Sometimes the cytoplasm of the cyst may retract from the cell wall.
G. duodenalis trophozoites in wet mounts.
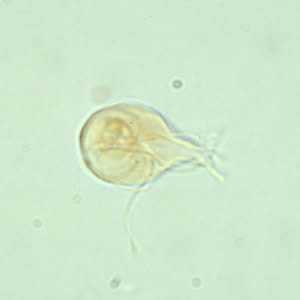
Figure A: G. duodenalis trophozoite in a wet mount stained with iodine.

Figure B: G. duodenalis trophozoite in a wet mount under differential interference contrast (DIC) microscopy. Image taken at 1000× magnification.
G. duodenalis trophozoites stained with trichrome.
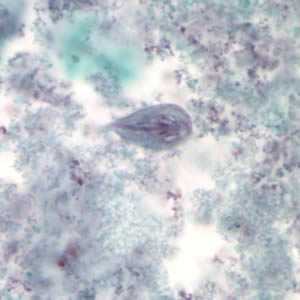
Figure A: G. duodenalis trophozoite stained with trichrome.
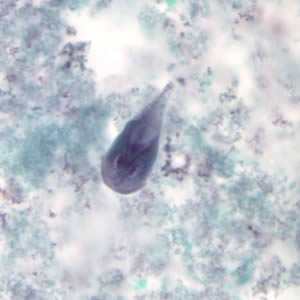
Figure B: G. duodenalis trophozoite stained with trichrome.
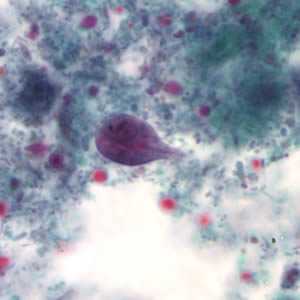
Figure C: Giardia duodenalis trophozoite stained with trichrome.
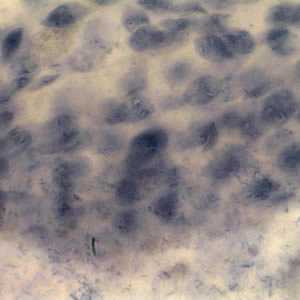
Figure D: G. duodenalis trophozoites. Image contributed by the Vermont Department of Health Laboratory.
G. duodenalis trophozoites in unique stains.

Figure A: G. duodenalis trophozoites in Kohn stain.

Figure B: G. duodenalis trophozoites in a Giemsa stained mucosal imprint
Cysts of Giardia duodenalis and oocysts of Cryptosporidium parvum.
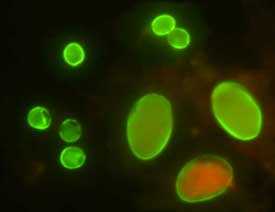
Figure A: Cysts of G. duodenalis (lower right) and oocysts of Cryptosporidium parvum (upper left) labeled with commercially available immunofluorescent antibodies.
Laboratory Diagnosis

Cysts of G. duodenalis (lower right) and Cryptosporidium (upper left) labeled with commercially available immunofluorescent antibodies.
Giardiasis is diagnosed by the identification of cysts or trophozoites in the feces, using direct mounts as well as concentration procedures. Cysts are typically seen in wet mount preparations, while trophozoites are seen in permanent mounts (i.e. trichrome). Repeated samplings may be necessary. In addition, samples of duodenal fluid (e.g., Enterotest) or duodenal biopsy may demonstrate trophozoites. Alternate methods for detection include antigen detection tests by enzyme immunoassays, and detection of parasites by immunofluorescence. Both methods are available in commercial kits.
Direct Immunofluorescence Assay (DFA)
A direct immunofluorescence assay (DFA) is available for diagnosing Giardia duodenalis infections. Antibodies tagged with fluorescent markers are added to stool and incubated. Visualization under a fluorescent microscope shows the Giardia cysts as green, glowing ovoid objects. This test includes antibodies for Cryptosporidium and both diseases can be tested for simultaneously.
Treatment Information
Several prescription drugs are available to treat giardiasis including metronidazole and tinidazole. Nitazoxanide has provided some encouraging results in the management of giardiasis in children.
DPDx is an education resource designed for health professionals and laboratory scientists. For an overview including prevention and control visit www.cdc.gov/parasites/.
- Page last reviewed: May 3, 2016
- Page last updated: May 3, 2016
- Content source:
- Global Health – Division of Parasitic Diseases and Malaria
- Notice: Linking to a non-federal site does not constitute an endorsement by HHS, CDC or any of its employees of the sponsors or the information and products presented on the site.
- Maintained By:


 ShareCompartir
ShareCompartir
 Laboratory Diagnosis of Giardiasis -- Giardia duodenalis
Laboratory Diagnosis of Giardiasis -- Giardia duodenalis