Dirofilariasis
[Dirofilaria immitis] [D. repens] [D. tenuis] [D. ursi]
Causal Agents
Zoonotic filarid nematodes in the genus Dirofilaria. The normal hosts for Dirofilaria spp. in nature are usually carnivores. The most commonly seen species in human patients are D. repens, D. tenuis, and D. immitis (the dog heartworm). Humans have also been infected with D. ursi, D. subdermata, and D. striata.
Life Cycles
Dirofilaria immitis
Dirofilaria repens
Dirofilaria tenuis
Dirofilaria ursi
Geographic Distribution
Dirofilaria immitis is cosmopolitan in dogs. Dirofilaria repens infects dogs and cats in the Old World, while D. tenuis infects raccoons in North America. Dirofilaria ursi and D. subdermata are also North American, infecting bears and porcupines, respectively. Dirofilaria striata is a parasite of wild felids in North, Central, and South America.
Clinical Presentation
Dirofilaria immitis causes pulmonary disease in humans. The parasite cannot develop in the human host and larvae that migrate to the heart usually die. Dead worms produce infarcts when they lodge in pulmonary vessels; these infarcts are usually referred to as "coin lesions". Following embolization, patients may present with chest pain, cough, fever, chill, malaise, and hemoptysis. There is often a mild eosinophilia. Other species of Dirofilaria usually manifest as subcutaneous nodules. These nodules are usually, tender, painful, and may be migratory. Adults of D. repens and D. tenuis are often found in the subconjunctiva.
Dirofilaria spp.
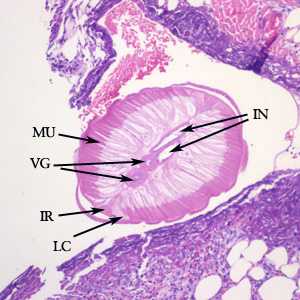
Figure A: Cross-section of Dirofilaria sp. from a subcutaneous nodule, stained with hematoxylin and eosin (H&E). Morphologic features visible in this image include tall, prominent muscle cells (MU), coiled vagina (VG), coiled intestine (IN), lateral chords (LC), and prominent internal lateral ridges (IR). Image courtesy of Drs. Dirk Elston and Paul Bourbeau.
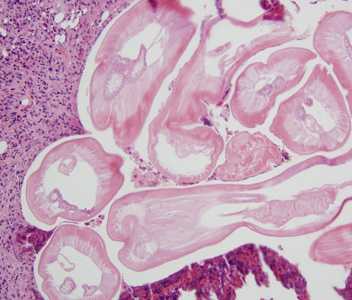
Figure B: Cross-sections of Dirofilaria spp. from a subcutaneous scalp nodule, stained with H&E. Image courtesy of the Department of Dermatopathology, University of Michigan, Ann Arbor, MI.
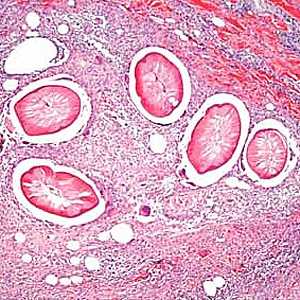
Figure C: Cross-sections of Dirofilaria sp. from a subcutaneous nodule above the right breast of a female patient who traveled to several western European countries, stained with H&E. Image taken at 100x magnification. Image courtesy of Dr. Truus Derks.
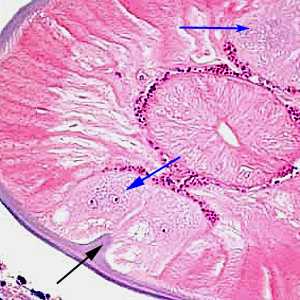
Figure D: Higher magnification of the same specimen as Figure C, taken at 400x magnification. Note the presence of lateral chords (blue arrows) and internal lateral ridge (black arrow).
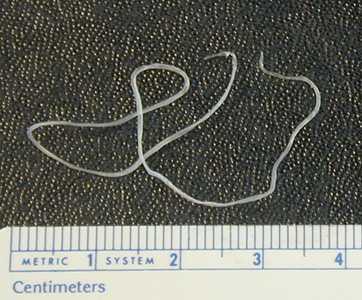
Figure E: Dirofilaria sp. (suspect D. tenuis) removed from the eye of a patient.

Figure F: Close-up of the specimen in Figure E showing the cuticular ridging. A uterine tube can also be seen through the cuticle.
Laboratory Diagnosis
Dirofilaria immitis is usually diagnosed by the finding of coin lesions on chest roentgenograms. The species that produce subcutaneous nodules are diagnosed by the finding of adult worms in biopsy specimens of the nodules. The morphologic features of the cuticle, musculature, and lateral chords are important criteria for identifying Dirofilaria. Worms removed from the eye are usually diagnosed by external features of the cuticle; worms may also be processed by routine histologic methods to study the internal structures. There are currently no serologic or molecular methods available for diagnosing human dirofilariasis in the U.S.
Treatment Information
The definitive treatment of Dirofilaria infection in humans is surgical removal of lung granulomas and subcutaneous nodules; this treatment is also curative. In many cases, no drug treatment is necessary.
DPDx is an education resource designed for health professionals and laboratory scientists. For an overview including prevention and control visit www.cdc.gov/parasites/.
- Page last reviewed: May 3, 2016
- Page last updated: May 3, 2016
- Content source:
- Global Health – Division of Parasitic Diseases and Malaria
- Notice: Linking to a non-federal site does not constitute an endorsement by HHS, CDC or any of its employees of the sponsors or the information and products presented on the site.
- Maintained By:


 ShareCompartir
ShareCompartir
 . In the definitive host, the L3 larvae undergo two more molts into L4 and adults. Adults reside in pulmonary arteries, and are occasionally found in the right ventricle of the heart
. In the definitive host, the L3 larvae undergo two more molts into L4 and adults. Adults reside in pulmonary arteries, and are occasionally found in the right ventricle of the heart  . Adult females are usually 230-310 mm long by 350 µm wide; males are usually 120-190 mm long by 300 µm wide. Adults can live for 5 - 10 years. In the heart, the female worms are capable of producing microfilariae over their lifespan. The microfilariae are found in peripheral blood
. Adult females are usually 230-310 mm long by 350 µm wide; males are usually 120-190 mm long by 300 µm wide. Adults can live for 5 - 10 years. In the heart, the female worms are capable of producing microfilariae over their lifespan. The microfilariae are found in peripheral blood  . A mosquito ingests the microfilariae during a blood meal
. A mosquito ingests the microfilariae during a blood meal  . After ingestion, the microfilariae migrate from the mosquito's midgut through the hemocoel to the Malpighian tubules in the abdomen
. After ingestion, the microfilariae migrate from the mosquito's midgut through the hemocoel to the Malpighian tubules in the abdomen  . There the microfilariae develop into first-stage larvae
. There the microfilariae develop into first-stage larvae  and subsequently into third-stage infective larvae
and subsequently into third-stage infective larvae  . The third-stage infective larvae migrate to the mosquito's proboscis
. The third-stage infective larvae migrate to the mosquito's proboscis  and can infect another definitive host when it takes a blood meal
and can infect another definitive host when it takes a blood meal  , D. immitis larvae tend to follow the same migratory pathway as in the canine host, ending up in the lungs, where they often lodge in small-caliber vessels, causing infarcts and typical "coin lesions" visible on radiographs.
, D. immitis larvae tend to follow the same migratory pathway as in the canine host, ending up in the lungs, where they often lodge in small-caliber vessels, causing infarcts and typical "coin lesions" visible on radiographs.
 , D. repens usually manifests as either a wandering worm in the subcutaneous tissue or a granulomatous nodule, although there are reports of pulmonary dirofilariasis with this species .
, D. repens usually manifests as either a wandering worm in the subcutaneous tissue or a granulomatous nodule, although there are reports of pulmonary dirofilariasis with this species .