
Dientamoeba fragilis Infection
[Dientamoeba fragilis]
Causal Agents
Despite its name, Dientamoeba fragilis is not an ameba but a flagellate. This protozoan parasite produces trophozoites; cysts have not been identified. Infection may be either symptomatic or asymptomatic.
Life Cycle
The complete life cycle of Dientamoeba fragilis has not yet been determined, and assumptions were made based on clinical data. Historically, this species was known only from the trophozoite stage in stools of infected individuals![]() . In 2014, cyst and precyst stages were described for the first time in clinical human specimens. These data are still considered preliminary and further testing should be done to validate the existence of this stage in the human host.
. In 2014, cyst and precyst stages were described for the first time in clinical human specimens. These data are still considered preliminary and further testing should be done to validate the existence of this stage in the human host.
D. fragilis is probably transmitted by fecal-oral route![]() and transmission via helminth eggs (e.g., Ascaris, Enterobius spp.) has been postulated
and transmission via helminth eggs (e.g., Ascaris, Enterobius spp.) has been postulated![]() . Trophozoites of D. fragilis have characteristically one or two nuclei (
. Trophozoites of D. fragilis have characteristically one or two nuclei (![]() ,
, ![]() ), and it is found in children complaining of intestinal (e.g., intermittent diarrhea, abdominal pain) and other symptoms (e.g., nausea, anorexia, fatigue, malaise, poor weight gain).
), and it is found in children complaining of intestinal (e.g., intermittent diarrhea, abdominal pain) and other symptoms (e.g., nausea, anorexia, fatigue, malaise, poor weight gain).
Reference: Stark D, Garcia LS, Barratt JLN, Phillips O, Roberts T, Marriot D, Harkness J, Ellis JT. Description of Dientamoeba fragilis cyst and precystic forms from human samples. Journ Clin Micro. 2014; 52: 2680-2683.
Geographic Distribution
Worldwide.
Clinical Presentation
Symptoms that have been associated with infection include diarrhea, abdominal pain, anorexia, nausea, vomiting, fatigue, and weight loss.
Dientamoeba fragilis binucleate trophozoites stained with trichrome
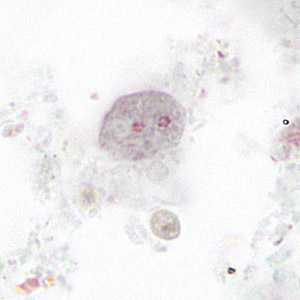
Figure A: Binucleate form of a trophozoite of D. fragilis, stained with trichrome.
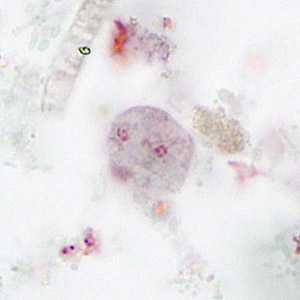
Figure B: Binucleate form of a trophozoite of D. fragilis, stained with trichrome.
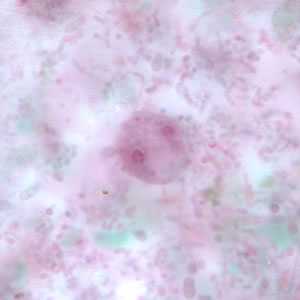
Figure E: Binucleate form of a trophozoite of D. fragilis, stained with trichrome.
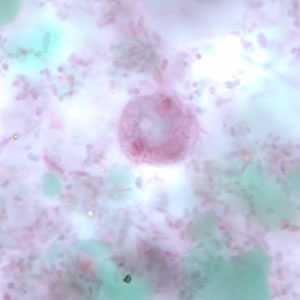
Figure D: Binucleate form of a trophozoite of D. fragilis, stained with trichrome.
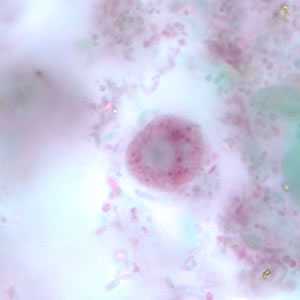
Figure C: Binucleate form of a trophozoite of D. fragilis, stained with trichrome.
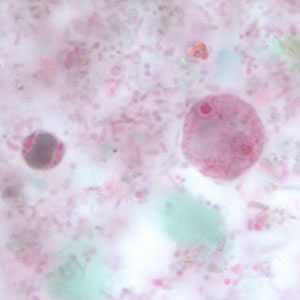
Figure F: Binucleate form of trophozoites of D. fragilis, stained with trichrome. A cyst-like form of Blastocystis hominis lies to the left of the D. fragilis.
Dientamoeba fragilis uninucleate trophozoites stained with trichrome.
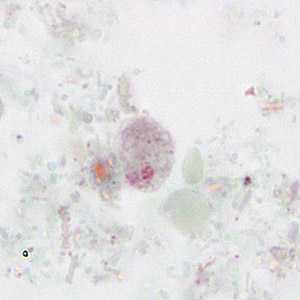
Figure A:Uninucleate form of a trophozoite of D. fragilis, stained with trichrome.
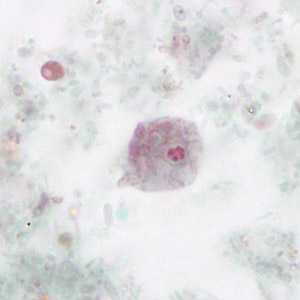
Figure B: Uninucleate form of a trophozoite of D. fragilis, stained with trichrome.
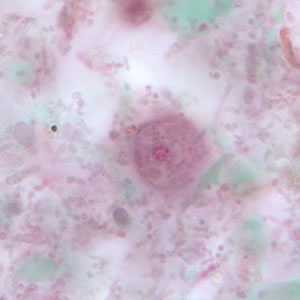
Figure C: Uninucleate form of a trophozoite of D. fragilis, stained with trichrome.
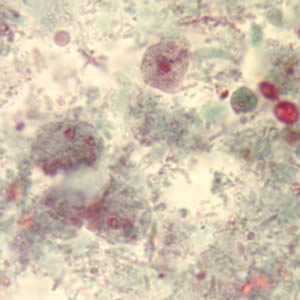
Figure D: Binucleate and uninucleate forms of trophozoites of D. fragilis, stained with trichrome.
Laboratory Diagnosis
Infection is diagnosed through detection of trophozoites in permanently stained fecal smears (e.g., trichrome). This parasite is not detectable by stool concentration methods. Dientamoeba fragilis trophozoites can be easily overlooked because they are pale-staining and their nuclei may resemble those of Endolimax nana or Entamoeba hartmanni.
Morphology
More on: Morphologic comparison with other intestinal parasites.
Treatment Information
Safe and effective drugs are available. The drug of choice is iodoquinol. Paromomycin*, tetracycline*, (contraindicated in children under age 8, pregnant and lactating women) or metronidazole can also be used.
* This drug is approved by the FDA, but considered investigational for this purpose.
DPDx is an education resource designed for health professionals and laboratory scientists. For an overview including prevention and control visit www.cdc.gov/parasites/.
- Page last reviewed: May 3, 2016
- Page last updated: May 3, 2016
- Content source:
- Global Health – Division of Parasitic Diseases and Malaria
- Notice: Linking to a non-federal site does not constitute an endorsement by HHS, CDC or any of its employees of the sponsors or the information and products presented on the site.
- Maintained By:


 ShareCompartir
ShareCompartir