Superior oblique myokymia
Superior oblique myokymia is a neurological disorder affecting vision and was named by Hoyt and Keane in 1970.[1]
| Superior oblique myokymia | |
|---|---|
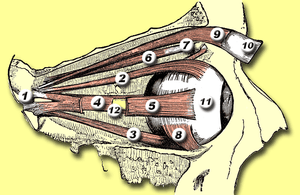 | |
| 6 = Superior oblique muscle | |
| Specialty | Neurology |
It is a condition that presents as repeated, brief episodes of movement, shimmering or shaking of the vision of one eye, a feeling of the eye trembling, or vertical/tilted vision. It can present as one or more of these symptoms. Diagnosis is most often made by the elimination of other conditions, disorders or diseases. Onset usually occurs in adulthood, and the course is benign and is not commonly associated with other disorders.


Causes
In 1983, Bringewald postulated that superior oblique myokymia resulted from vascular compression of the trochlear nerve (fourth cranial nerve), which controls the action of the superior oblique muscle in the eye.[2] By 1998, there had been only one reported case of compression of the trochlear nerve by vessels.[3][4] More recently, magnetic resonance imaging experiments have shown that neurovascular compression at the root exit zone of the trochlear nerve can result in superior oblique myokymia.[5]
Diagnosis
Treatment
Treatment can include pharmaceutical or surgical means. The drug carbamazepine (Tegretol) has been used successfully. Other drugs used with variable success include gabapentin and, recently, memantine. Successful surgery options include superior oblique tenectomy accompanied by inferior oblique myectomy.[6] However, "Overall, the bulk of the ophthalmic literature would agree with the viewpoint that invasive craniotomy surgical procedures should be justified only by the presence of intractable and absolutely unbearable symptoms."[7]
Samii et al.[3] and Scharwey and Samii[4] described a patient who had superior oblique myokymia for 17 years. The interposition of a Teflon pad between the trochlear nerve and a compressing artery and vein at the nerve's exit from the midbrain led to a remission lasting for a follow-up of 22 months.
References
- Hoyt WF, Keane JR (October 1970). "Superior oblique myokymia. Report and discussion on five cases of benign intermittent uniocular microtremor". Arch. Ophthalmol. 84 (4): 461–7. doi:10.1001/archopht.1970.00990040463011. PMID 5492451.
- Bringewald PR (August 1983). "Superior oblique myokymia". Arch. Neurol. 40 (8): 526. doi:10.1001/archneur.1983.04210070066021. PMID 6870617.
- Samii M, Rosahl SK, Carvalho GA, Krzizok T (1998). "Microvascular decompression for superior oblique myokymia: first experience. Case report". J. Neurosurg. 89 (6): 1020–4. doi:10.3171/jns.1998.89.6.1020. PMID 9833830.
- Scharwey K, Krzizok T, Samii M, Rosahl SK, Kaufmann H (2000). "Remission of superior oblique myokymia after microvascular decompression". Ophthalmologica. 214 (6): 426–8. doi:10.1159/000027537. PMID 11054004.
- Yousry I, Dieterich M, Naidich TP, Schmid UD, Yousry TA (March 2002). "Superior oblique myokymia: magnetic resonance imaging support for the neurovascular compression hypothesis". Ann. Neurol. 51 (3): 361–8. doi:10.1002/ana.10118. PMID 11891831.
- "Superior Oblique Myokymia 379.58". Retrieved 2007-06-25.
- J Optom 2014;7:68-74 - Vol. 7 Num.2 DOI: 10.1016/j.optom.2013.06.004