Radial neuropathy
Radial neuropathy is a type of mononeuropathy which results from acute trauma to the radial nerve that extends the length of the arm.[2] It is known as transient paresthesia when sensation is temporarily abnormal.[3]
| Radial neuropathy | |
|---|---|
| Other names | Radial mononeuropathy |
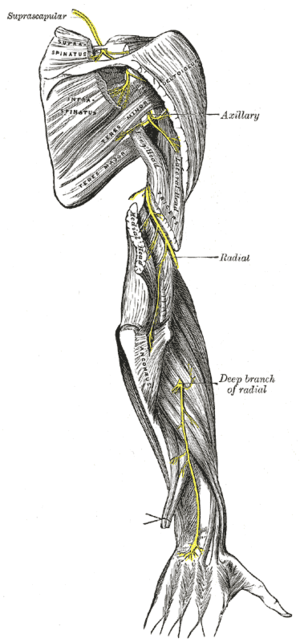 | |
| The suprascapular, axillary, and radial nerves. | |
| Specialty | Neurology |
| Causes | Broken bone, Direct nerve injury[1] |
| Diagnostic method | MRI, Ultrasound[2] |
| Treatment | Corticosteroid, Pain medication[1] |
Signs and symptoms
Symptoms of radial neuropathy vary depending on the severity of the trauma; however, common symptoms may include wrist drop, numbness on the back of the hand and wrist, and inability to voluntarily straighten the fingers. Loss of wrist extension is due to loss of the ability to move of the posterior compartment of forearm muscles.[2][4] In the event of lacerations to the wrist area the symptom would therefore be sensory. Additionally, depending on the type of trauma, other nerves may be affected such as the median nerve and axillary nerves.[5]
Causes
There are many ways to acquire radial nerve neuropathy, including:[6]
- Upper arm - a fracture of the bone
- Elbow - entrapment of the nerve
- Wrist - elbow deformity and soft-tissue masses
- Axilla - here the most common cause is compression. However, a dislocation of the humerus is a possible factor as well. It could also be due to brachial plexus compression.
Mechanism
The mechanism of radial neuropathy is such that it can cause focal demyelination and axonal degeneration.[7] These would be caused via laceration or compression of the nerve in question.[8]
Diagnosis
Radial neuropathy may be diagnosed using MRI, ultrasound, nerve conduction study or electromyography (EMG).[2]
Treatment

The treatment and management of radial neuropathy can be achieved via the following methods:[2][9][10]
- Physical therapy or occupational therapy
- Surgery (depending on the specific area and extent of damage)
- Tendon transfer (the origin remains the same but insertion is moved)
Prognosis
Radial neuropathy is not necessarily permanent, though there could be partial loss of movement or sensation. Complications include deformity of the hand in some individuals.[1] If the injury is axonal (the underlying nerve fiber itself is damaged), recovery may take months or years and full recovery may never occur. EMG and nerve conduction studies are typically performed to diagnose the extent and distribution of the damage, and to help with prognosis for recovery.
Culture and society
There are a number of terms used to describe radial nerve injuries, which are dependent on the causation factor such as:
- Honeymoon palsy from another individual sleeping on and compressing one's arm overnight.[11]
- Saturday night palsy from falling asleep with one's arm hanging over the arm rest of a chair, compressing the radial nerve.[12]
- Squash palsy, from traction forces associated with the sport squash, happens to squash players during periods between matches.[13]
See also
References
- "Radial nerve dysfunction: MedlinePlus Medical Encyclopedia". medlineplus.gov. NIH. Retrieved 10 September 2016.
- "Radial Mononeuropathy: Background, Pathophysiology, Epidemiology". Mdscape. eMedicine. Retrieved 16 August 2016.
- "Paresthesia Information Page: National Institute of Neurological Disorders and Stroke (NINDS)". www.ninds.nih.gov. Archived from the original on 2 December 2016. Retrieved 18 August 2016.
- Han, Bo Ram; Cho, Yong Jun; Yang, Jin Seo; Kang, Suk Hyung; Choi, Hyuk Jai (1 March 2014). "Clinical Features of Wrist Drop Caused by Compressive Radial Neuropathy and Its Anatomical Considerations". Journal of Korean Neurosurgical Society. 55 (3): 148–151. doi:10.3340/jkns.2014.55.3.148. ISSN 2005-3711. PMC 4024814. PMID 24851150.
- Frontera, Walter R.; Silver, Julie K.; Jr, Thomas D. Rizzo (2014-09-05). Essentials of Physical Medicine and Rehabilitation. Elsevier Health Sciences. p. 129. ISBN 9780323222723. Retrieved 10 September 2016.
- "Radial Nerve Lesion (C5-C8) Professional Reference | Patient". Patient. Retrieved 10 September 2016.
- Wang, Jack T.; Medress, Zachary A.; Barres, Ben A. (9 January 2012). "Axon degeneration: Molecular mechanisms of a self-destruction pathway". The Journal of Cell Biology. 196 (1): 7–18. doi:10.1083/jcb.201108111. ISSN 0021-9525. PMC 3255986. PMID 22232700. Retrieved 10 September 2016.
- Micheo, [edited by] William (2010). Musculoskeletal, Sports and Occupational Medicine. New York: Demos Medical Pub., LLC. p. 192. ISBN 9781617050077. Retrieved 10 September 2016.CS1 maint: extra text: authors list (link)
- "Tendon Transfers: History, Concepts, Timing of Tendon Transfer". 2017-05-02. Cite journal requires
|journal=(help) - Wolfe, Scott W.; Pederson, William C.; Hotchkiss, Robert N.; Kozin, Scott H.; Cohen, Mark S. (2010-11-24). Green's Operative Hand Surgery: Expert Consult: Online and Print. Elsevier Health Sciences. p. 1078. ISBN 978-1455737413. Retrieved 10 September 2016.
- Ebnezar, John (2010). Textbook of Orthopedics. JP Medical Ltd. p. 342. ISBN 978-81-8448-744-2.
- Goodman, Catherine C.; Fuller, Kenda S. (2011-02-14). Pathology for the Physical Therapist Assistant. Elsevier Health Sciences. p. 890. ISBN 978-1437708936.
- "Medscape /Axillary Nerve Injury Associated With Sports". www.medscape.com. Retrieved 10 September 2016.
Further reading
- Cartwright, Michael S.; Yoon, Joon Shik; Lee, Kyu Ho; Deal, Nicole; Walker, Francis O. (1 April 2011). "Diagnostic Ultrasound for Traumatic Radial Neuropathy". American Journal of Physical Medicine & Rehabilitation. 90 (4): 342–343. doi:10.1097/PHM.0b013e3181e29daa. ISSN 0894-9115. PMC 2964388. PMID 20531154.
- Tuncel, Umut; Turan, Aydin; Kostakoglu, Naci (1 January 2011). "Acute closed radial nerve injury". Asian Journal of Neurosurgery. 6 (2): 106–109. doi:10.4103/1793-5482.92175. ISSN 1793-5482. PMC 3277063. PMID 22347334.
External links
| Classification | |
|---|---|
| External resources |