Low birth weight
Low birth weight (LBW) is defined by the World Health Organization as a birth weight of a infant of 2,499 g or less, regardless of gestational age.[1] Subcategories include very low birth weight (VLBW), which is less than 1500 g (3 pounds 5 ounces), and extremely low birth weight (ELBW), which is less than 1000 g (2 pounds 3 ounces).[2] Normal weight at term delivery is 2500–4200 g (5 pounds 8 ounces – 9 pounds 4 ounces).
Causes
LBW is either caused by preterm birth (that is, a low gestational age at birth, commonly defined as younger than 37 weeks of gestation) or the infant being small for gestational age (that is, a slow prenatal growth rate), or a combination of both.
In general, risk factors in the mother that may contribute to low birth weight include young ages, multiple pregnancies, previous LBW infants, poor nutrition, heart disease or hypertension, untreated coeliac disease, drug addiction, alcohol abuse, and insufficient prenatal care. Environmental risk factors include smoking, lead exposure, and other types of air pollutions.[3][4][5]
Preterm birth
Four different pathways have been identified that can result in preterm birth and have considerable evidence: precocious fetal endocrine activation, uterine overdistension, decidual bleeding, and intrauterine inflammation/infection.[6] From a practical point a number of factors have been identified that are associated with preterm birth, however, an association does not establish causality.
Being small for gestational age
Being small for gestational age can be constitutional, that is, without an underlying pathological cause, or it can be secondary to intrauterine growth restriction, which, in turn, can be secondary to many possible factors. For example, babies with congenital anomalies or chromosomal abnormalities are often associated with LBW. Problems with the placenta can prevent it from providing adequate oxygen and nutrients to the fetus. Infections during pregnancy that affect the fetus, such as rubella, cytomegalovirus, toxoplasmosis, and syphilis, may also affect the baby's weight.
Environmental factors
While active maternal tobacco smoking has well established adverse perinatal outcomes such as LBW, that mothers who smoke during pregnancy are twice as likely to give birth to low-birth weight infants. Review on the effects of passive maternal smoking, also called environmental tobacco exposure (ETS), demonstrated that increased risks of infants with LBW were more likely to be expected in ETS-exposed mothers.[7][8]
Regarding environmental toxins in pregnancy, elevated blood lead levels in pregnant women, even those well below 10 ug/dL can cause miscarriage, premature birth, and LBW in the offspring. With 10 ug/dL as the Centers for Disease Control and Prevention's “level of concern”, this cut-off value really needs to arise more attentions and implementations in the future.[9]
The combustion products of solid fuel in developing countries can cause many adverse health issues in people. Because a majority of pregnant women in developing countries, where rate of LBW is high, are heavily exposed to indoor air pollution, increased relative risk translates into substantial population attributable risk of 21% of LBW.[10]
The potentially harmful effects of air pollution are particularly concerning given the pervasiveness of air pollution. The exact mechanism by which air pollution affects fetuses is unknown, but it is suggested that air pollutants enter the body through direct diffusion or active transport.[11] Once in the body, it is thought that air pollutants affect birth outcomes by oxidative stress, changes in hemodynamic factors, disruption of endocrine systems, and finally with genetic and epigenetic changes[12].
One environmental exposure which has been found to increase the risk of low birth weight is particulate matter, a component of ambient air pollution.[13] Because particulate matter is composed of extremely small particles, even nonvisible levels can be inhaled and present harm to the fetus.[14] Particulate matter exposure can cause inflammation, oxidative stress, endocrine disruption, and impaired oxygen transport access to the placenta,[15] all of which are mechanisms for heightening the risk of low birth weight.[16] When inhaled, particles smaller than 1 µm can penetrate the alveolar wall, enter the maternal bloodstream so that particles and inflammatory mediators cross the placenta, and reach the fetus[17]. Some studies have indicated that PM2.5 exposure during the second trimester may lead to the strongest effects on low birth weight[18]. To reduce exposure to particulate matter, pregnant women can monitor the EPA’s Air Quality Index and take personal precautionary measures such as reducing outdoor activity on low quality days, avoiding high-traffic roads/intersections, and/or wearing personal protective equipment (i.e., facial mask of industrial design). Indoor exposure to particulate matter can also be reduced through adequate ventilation, as well as use of clean heating and cooking methods.[19][20]
Other environmental exposures that have been shown to increase the rates of low birth weight are compounds that are associated with traffic-related pollution, most significantly, nitrogen dioxide (NO2). Nitrogen dioxide is often used as an indicator of traffic-related air pollution[21]. Stieb et al. used national data to study the association between nitrogen dioxide exposure and pregnancy outcomes in 2.5 million births in Canada between 1999 and 2008 using land use regression models to estimate nitrogen dioxide concentrations[21]. They found that exposure to nitrogen dioxide was associated with 4% higher odds of giving birth to a child that is small for gestational age [21]. Even after the researchers adjusted for neighborhood socioeconomic factors, there was still a strong association between nitrogen dioxide and low birth weight [21]. This research also showed evidence of a dose-response relationship, meaning that more exposure to nitrogen dioxide an expectant mother was exposed to, the higher the likelihood of giving birth to a low birth weight child [21].
The association between traffic related pollution and low birth weight has been observed in multiple studies conducted in different parts of the world. Généreux et al. studied a population of Canadian women and found that living close to highways is associated with adverse birth outcomes, even among women considered high socioeconomic status[22]. Ghosh et al. examined 4 air toxin monitoring stations in Los Angeles, California, and found that the odds of a low birth weight child increased by 2-5% when mothers were exposed to nitric oxide, nitrogen dioxide, and nitrogen oxides[23]. Furthermore, these researchers found that traffic exhaust leads to low birth weight in long-term and short-term exposure, especially in the third trimester [24]. In a study of Swedish newborn children, researchers used ultrasound techniques to show that exposure to nitrogen oxides consistently and negatively affected fetal growth late in pregnancy (after 7 months). Furthermore, they found that the population that was affected had relatively low exposures, which were generally below WHO air quality guidelines [17].
Another measure of air pollution is exposure to polycyclic aromatic hydrocarbons from motor vehicle exhaust, which has been associated with a 1-3% increased odds of low birth weight [25]. It is hypothesized that hydrocarbons, which can cross into the placenta, have antiestrogenic effects and also cause DNA damage that leads to apoptosis or cell death [26].
A correlation between maternal exposure to CO and low birth weight has been reported that the effect on birth weight of increased ambient CO was as large as the effect of the mother smoking a pack of cigarettes per day during pregnancy.[27] It has been revealed that adverse reproductive effects (e.g., risk for LBW) were correlated with maternal exposure to air pollution combustion emissions in Eastern Europe and North America.[28] Mercury is a known toxic heavy metal that can harm fetal growth and health, and there has been evidence showing that exposure to mercury (via consumption of large oily fish) during pregnancy may be related to higher risks of LBW in the offspring.[29]
It has also been hypothesized that another air pollutant, ozone, can cause low birth weight. While ozone has been associated with preterm delivery, studies linking ozone and low birth weight have been inconsistent [30]. Some have shown a positive association between the two, others have shown no association, and some have found that ozone may actually be a protective factor against low birth weight[31]. This last phenomenon is potentially explained by studies that have shown that ozone can activate an antioxidant system, which may help bring oxygen to tissues [32].
It was revealed that, exposure of pregnant women to airplane noise was found to be associated with low birth weight. Aircraft noise exposure caused adverse effects on fetal growth leading to low birth weight and preterm infants.[33][34]
Periodontal health
Low birthweight, pre-term birth and pre-eclampsia have been associated with maternal periodontitis exposure. But the strength of the observed associations is inconsistent and vary according to the population studied, the means of periodontal assessment and the periodontal disease classification employed.[35] However the best is that the risk of low birth weight can be reduced with very simple therapy. Treatment of periodontal disease during gestation period is safe and reduction in inflammatory burden reduces the risk of preterm birth as well as low birth weight.[36]
Effects
LBW is closely associated with fetal and Perinatal mortality and Morbidity, inhibited growth and cognitive development, and chronic diseases later in life. At the population level, the proportion of babies with a LBW is an indicator of a multifaceted public-health problem that includes long-term maternal malnutrition, ill health, hard work and poor health care in pregnancy. On an individual basis, LBW is an important predictor of newborn health and survival and is associated with higher risk of infant and childhood mortality.[37]
Low birth weight constitutes as sixty to eighty percent of the infant mortality rate in developing countries. Infant mortality due to low birth weight is usually directly causal, stemming from other medical complications such as preterm birth, poor maternal nutritional status, lack of prenatal care, maternal sickness during pregnancy, and an unhygienic home environment.[38][39] According to an analysis by University of Oregon, reduced brain volume in children is also tied to low birth-weight.[40][41]
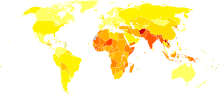
Epidemiology
A study by the Agency for Healthcare Research and Quality (AHRQ) found that of the 3.8 million births that occurred in the United States in 2011, approximately 6.1% (231,900) were diagnosed with low birth weight (<2,500 g). Approximately 49,300 newborns (1.3%) weighed less than 1,500 grams (VLBW).[42] Infants born at low birth weight are at a higher risk for developing neonatal infection.
References
- P07 - Disorders related to short gestation and low birth weight in ICD-10
- "eMedicine - Extremely Low Birth Weight Infant : Article by KN Siva Subramanian, MD". Retrieved 2007-11-28.
- "Labor and delivery - Low Birth Weight". Umm.edu. 2008-10-22. Retrieved 2011-01-05.
- Tersigni, C.; Castellani, R.; de Waure, C.; Fattorossi, A.; De Spirito, M.; Gasbarrini, A.; Scambia, G.; Di Simone, N. (2014). "Celiac disease and reproductive disorders: meta-analysis of epidemiologic associations and potential pathogenic mechanisms". Human Reproduction Update. 20 (4): 582–593. doi:10.1093/humupd/dmu007. ISSN 1355-4786. PMID 24619876.
- Saccone G, Berghella V, Sarno L, Maruotti GM, Cetin I, Greco L, Khashan AS, McCarthy F, Martinelli D, Fortunato F, Martinelli P (Oct 9, 2015). "Celiac disease and obstetric complications: a systematic review and metaanalysis". Am J Obstet Gynecol. 214 (2): 225–34. doi:10.1016/j.ajog.2015.09.080. PMID 26432464.
- Simhan HN, Caritis SN (2007). "Prevention of Preterm Delivery". New England Journal of Medicine. 357 (5): 477–487. doi:10.1056/NEJMra050435. PMID 17671256.
- Knopik VS. Maternal smoking during pregnancy and child outcomes: real or spurious effect? Dev Neuropsychol. 2009;34(1):1-36.
- Salmasi G, Grady R, Jones J, et al. Environmental tobacco smoke exposure and perinatal outcomes: a systematic review and meta-analyses. Acta Obstet Gynecol Scand. 2010;89(4):423-41.
- Cleveland LM, Minter ML, Cobb KA, et al. Lead hazards for pregnant women and children: part 1: immigrants and the poor shoulder most of the burden of lead exposure in this country. Part 1 of a two-part article details how exposure happens, whom it affects, and the harm it can do. Am J Nurs. 2008 Oct;108(10):40-9
- Pope DP, Mishra V, Thompson L, et al. Risk of low birth weight and stillbirth associated with indoor air pollution from solid fuel use in developing countries. Epidemiol Rev. 2010 Apr;32(1):70-81
- Ha, S., Hu, H., Roussos-Ross, D., Haidong, K., Roth, J., & Xu, X. (October 2014). "The effects of air pollution on adverse birth outcomes". Environmental Research. 134: 198–204. doi:10.1016/j.envres.2014.08.002. PMC 4262551. PMID 25173052.CS1 maint: multiple names: authors list (link)
- Ha, S., Hu, H., Roussos-Ross, D., Haidong, K., Roth, J., & Xu, X. (October 2014). "The effects of air pollution on adverse birth outcomes". Environmental Research. 134: 198–204. doi:10.1016/j.envres.2014.08.002. PMC 4262551. PMID 25173052.CS1 maint: multiple names: authors list (link)
- EPA, OAR, US (2014-04-09). "Criteria Air Pollutants". www.epa.gov. Retrieved 2017-03-31.
- "CDC - Air Quality - Particle Pollution". www.cdc.gov. Retrieved 2017-03-31.
- Erickson, Anders C.; Arbour, Laura (2014-11-26). "The Shared Pathoetiological Effects of Particulate Air Pollution and the Social Environment on Fetal-Placental Development". Journal of Environmental and Public Health. 2014: 901017. doi:10.1155/2014/901017. ISSN 1687-9805. PMC 4276595. PMID 25574176.
- Lee, Pei-Chen; Talbott, Evelyn O.; Roberts, James M.; Catov, Janet M.; Bilonick, Richard A.; Stone, Roslyn A.; Sharma, Ravi K.; Ritz, Beate (2012-08-01). "Ambient air pollution exposure and blood pressure changes during pregnancy". Environmental Research. 117: 46–53. Bibcode:2012ER....117...46L. doi:10.1016/j.envres.2012.05.011. PMC 3656658. PMID 22835955.
- Malmqvist, E., Liew, Z., Källén, K., Rignell-Hydbom, A., Rittner, R., Rylander, L., & Ritz, B. (2017). "Fetal growth and air pollution - A study on ultrasound and birth measures". Environmental Research. 152: 73–80. doi:10.1016/j.envres.2016.09.017. PMID 27741452.CS1 maint: multiple names: authors list (link)
- Ha, S., Hu, H., Roussos-Ross, D., Haidong, K., Roth, J., & Xu, X (October 2014). "The effects of air pollution on adverse birth outcomes". Environmental Research. 134: 198–204. doi:10.1016/jenvres.2014.08.002 (inactive 2019-12-03).CS1 maint: multiple names: authors list (link)
- "Particulate matter". EPA. May 19, 2009.
- Group, US EPA National Center for Environmental Assessment, Research Triangle Park Nc, Environmental Media Assessment; Sacks, Jason. "2009 Final Report: Integrated Science Assessment for Particulate Matter". cfpub.epa.gov. Retrieved 2017-03-31.
- Stieb, David M; Chen, Li; Hystad, Perry; Beckerman, Bernardo S.; Jerrett, Michael; Tjepkema, Michael; Crouse, Daniel; Omariba, D. Walter; Peters, Paul A.; van DonKelaar, Aaron; Martin, Randall; Burnett, Richard; Liu, Shiliang; Smith-Doiron, Marc; Dugandzic, Rose (May 2016). "A national study of the association between traffic-related air pollution and adverse pregnancy outcomes in Canada, 1999-2008". Environmental Research. 148: 513–526. doi:10.1016/j.envres.2016.04.025.
- Généreux, M., Auger, N., Goneau, M., & and Daniel, M. (August 2008). "Neighbourhood socioeconomic status, maternal education and adverse birth outcomes among mothers living near highways". Journal of Epidemiology and Community Health. 62 (8): 695–700. doi:10.1136/jech.2007.066167. JSTOR 40665884.CS1 maint: multiple names: authors list (link)
- Ghosh, J. K., Wilhelm, M., Su, J., Goldberg, D., Cockburn, M., Jerrett, M., & and Ritz, B. (2012). "Assessing the Influence of Traffic-related Air Pollution on Risk of Term Low Birth Weight on the Basis of Land-Use-based Regression Models and Measures of Air Toxics". American Journal of Epidemiology. 175 (12): 1262–1274. doi:10.1093/aje/kwr469. PMID 22586068.CS1 maint: multiple names: authors list (link)
- Ghosh, J. K., Wilhelm, M., Su, J., Goldberg, D., Cockburn, M., Jerrett, M., & and Ritz, B. (2012). "Assessing the Influence of Traffic-related Air Pollution on Risk of Term Low Birth Weight on the Basis of Land-Use-based Regression Models and Measures of Air Toxics". American Journal of Epidemiology. 175 (12): 1262–1274. doi:10.1093/aje/kwr469. PMID 22586068.CS1 maint: multiple names: authors list (link)
- Ghosh, J. K., Wilhelm, M., Su, J., Goldberg, D., Cockburn, M., Jerrett, M., & and Ritz, B. (2012). "Assessing the Influence of Traffic-related Air Pollution on Risk of Term Low Birth Weight on the Basis of Land-Use-based Regression Models and Measures of Air Toxics". American Journal of Epidemiology. 175 (12): 1262–1274. doi:10.1093/aje/kwr469. PMID 22586068.CS1 maint: multiple names: authors list (link)
- Ghosh, J. K., Wilhelm, M., Su, J., Goldberg, D., Cockburn, M., Jerrett, M., & and Ritz, B. (2012). "Assessing the Influence of Traffic-related Air Pollution on Risk of Term Low Birth Weight on the Basis of Land-Use-based Regression Models and Measures of Air Toxics". American Journal of Epidemiology. 175 (12): 1262–1274. doi:10.1093/aje/kwr469. PMID 22586068.CS1 maint: multiple names: authors list (link)
- Lewtas J. Air pollution combustion emissions: characterization of causative agents and mechanisms associated with cancer, reproductive, and cardiovascular effects. Mutat Res. 2007 Nov-Dec;636(1-3):95-133.
- Townsend CL, Maynard RL (Oct 2002). "Effects on health of prolonged exposure to low concentrations of carbon monoxide". Occup Environ Med. 59 (10): 708–11. doi:10.1136/oem.59.10.708. PMC 1740215. PMID 12356933.
- Gochfeld M, Burger J (Aug 2005). "Good fish/bad fish: a composite benefit-risk by dose curve". Neurotoxicology. 26 (4): 511–20. doi:10.1016/j.neuro.2004.12.010. PMID 15979722.
- Ha, S., Hu, H., Roussos-Ross, D., Haidong, K., Roth, J., & Xu, X. (October 2014). "The effects of air pollution on adverse birth outcomes". Environmental Research. 134: 198–204. doi:10.1016/j.envres.2014.08.002. PMC 4262551. PMID 25173052.CS1 maint: multiple names: authors list (link)
- Ha, S., Hu, H., Roussos-Ross, D., Haidong, K., Roth, J., & Xu, X. (October 2014). "The effects of air pollution on adverse birth outcomes". Environmental Research. 134: 198–204. doi:10.1016/j.envres.2014.08.002. PMC 4262551. PMID 25173052.CS1 maint: multiple names: authors list (link)
- Ha, S., Hu, H., Roussos-Ross, D., Haidong, K., Roth, J., & Xu, X. (October 2014). "The effects of air pollution on adverse birth outcomes". Environmental Research. 134: 198–204. doi:10.1016/j.envres.2014.08.002. PMC 4262551. PMID 25173052.CS1 maint: multiple names: authors list (link)
- Kawada T (Feb 2004). "The effect of noise on the health of children". J Nippon Med SCH. 71 (1): 5–10. doi:10.1272/jnms.71.5. PMID 15129589.
- Matsui T, Matsuno T, Ashimine K, et al. (Sep 2003). "Association between the rates of low birth-weight and/or preterm infants and aircraft noise exposure". Nippon Eiseigaku Zasshi. 58 (3): 385–94. doi:10.1265/jjh.58.385. PMID 14533568.
- Sanz, M (April 2013). "Periodontitis and adverse pregnancy outcomes: consensus report of the Joint EFP/AAP Workshop on Periodontitis and Systemic Diseases". J Periodontol. 84 (4 suppl): S164–9. doi:10.1902/jop.2013.1340016. PMID 23631576.
- Shah, Monali (November 2013). "Effect of nonsurgical periodontal therapy during gestation period on adverse pregnancy outcome: a systematic review". J Matern Fetal Neonatal Med. 26 (17): 1691–5. doi:10.3109/14767058.2013.799662. PMID 23617740.
- Stevens-Simon C, Orleans M (Sep 1999). "Low-birthweight prevention programs: the enigma of failure". Birth. 26 (3): 184–91. doi:10.1046/j.1523-536x.1999.00184.x. PMID 10655819.
- Andrews, K.M.; Brouillette, D.B; Brouillette, R.T. (2008). "Mortality, Infant". Encyclopedia of Infant and Early Childhood Development. Encyclopedia of Infant and Early Childhood Development. pp. 343–359. doi:10.1016/B978-012370877-9.00084-0. ISBN 9780123708779.
- Norton, M (2005). "New evidence on birth spacing: promising findings for improving newborn, infant, child, and maternal health". International Journal of Gynecology & Obstetrics. 89: S1–S6. doi:10.1016/j.ijgo.2004.12.012. PMID 15820364.
- "Baby Weight Growth Chart". Retrieved 2013-09-22.
- "Reduced brain volume in kids with low birth-weight tied to academic struggles, University of Oregon". 2013-06-10. Retrieved 2013-09-22.
- Kowlessar N.M., Jiang H.J., and Steiner C. Hospital Stays for Newborns, 2011. HCUP Statistical Brief #163. October 2013. Agency for Healthcare Research and Quality, Rockville, MD.