Hypodontia
Hypodontia is defined as the developmental absence of one or more teeth (excluding the third molars) which can affect both the primary and permanent dentition.[1] It is the most common developmental dental anomaly and can be challenging to manage clinically.[2] The term hypodontia is used to describe the whole range of the disorder from one missing tooth to the complete absence of all teeth, anodontia.
| Hypodontia | |
|---|---|
| Clinical photograph of a hypodontia case of missing upper lateral incisors | |
| Specialty | Dentistry |
Terminology in use varies. One text [3] has proposed the following descriptive terms:
- Hypodontia: A developmental or congenital condition characterised by fewer than normal teeth.
- Severe hypodontia: A developmental or congenital condition characterised by absence of 6 or more teeth.
- Oligodontia: A developmental or congenital condition characterised by fewer than normal teeth in the presence of systemic manifestations.
- Anodontia: a developmental or congenital condition characterised by absence of all teeth.
The descriptive terms agenesis or multiple dental agenesis are often used in the US.[3]
Individuals with hypodontia often exhibit other dental anomalies such as microdontia,[4][5] impaction of permanent canines [6] and transposition.[7]
Supernumerary teeth are teeth present in addition to the normal complement. This can occur in both dentitions.
Signs and symptoms
Most people with hypodontia are only missing one or two teeth, but can vary from one missing tooth to a full missing dentition.
The teeth most likely to be missing are permanent 2nd premolars and upper lateral incisors.[8]
Deciduous dentition
In the deciduous dentition the teeth most likely to be missing are upper laterals and lower central incisors, these account for about 50-90% of affected deciduous teeth.
It is most common for the missing teeth to be unilateral and agenesis only affecting one or two teeth.[8]
Permanent dentition
In the permanent dentition, the teeth most likely to be missing are the lower 2nd premolars and the upper lateral incisors. This pattern seems to vary more in individuals that have hypodontia as part of a syndrome.[8]
Dental features
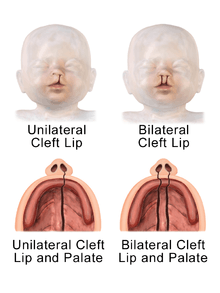
Most of the time tooth agenesis is not associated with a syndrome but it is a common feature in cleft-lip or cleft-lip and palate patients, particularly individuals with more severe clefts.[9] In these cases, agenesis often presents in the upper lateral incisor.
Examples of more conditions that may present with hypodontia as one of their features include Down Syndrome[10] and ectodermal dysplasia.[11]
It is known that hypodontia can contribute to abnormal occlusion, especially in its more severe cases, and also has linked to developmental delays, microdontia, taurodontia, enamel hypoplasia and ectopic positioning of permanent teeth due to the inability of neighbouring teeth to guide eruption.[12] It has been reported that 50% of patients with a canine/first premolar transposition also experience hypodontia, there are suggestions that this may be due to a genetic link.
Skeletal features
The skeletal features and growth patterns associated with hypodontia are unknown although there is some evidence to suggest that the cranio-facial features of individuals with missing teeth are different from those with a full natural dentition. Patients with hypodontia commonly present with a smaller lower anterior face height and lip protrusion which are linked with lower mandibular plane angles. Smaller lengths of maxilla and mandible and a Class III skeletal base are also associated with hypodontia. The tendency of the patient to have these skeletal effects becomes more significant as the severity of agenesis increases, especially when more than one type of tooth is missing.[13] Patients may appear over-closed due to the short face height and large freeway space associated with hypodontia.
Children
Studies suggest that children with mild hypodontia do have significant associated skeletal and dental features. It was found that it was associated with; a high-angle cranio-facial pattern, a class III malocclusion (in maxillary hypodontia) and a significant reduction in posterior facial height (with posterior and mandibular hypodontia).[14]
Associated anomalies
- Conical shaped teeth
- Ectopic canines
- Cleft lip and palate
- Diastema
- Delayed eruption
Cause
Several theories regarding the aetiology of hypodontia have been proposed in existing literature. There have been various theories mostly looking into genetic and environmental aspects and how they may both be involved.[8] However, the exact cause remains unclear. The extent of individual influences of genetic and environmental factors is still widely debated.[2]
These theories can be categories into evolutional or anatomical.[16]
Preliminary studies focused on an evolutionary approach which suggested shortening of the intermaxillary complex and thus shorter arches may contribute to a decrease in number of teeth. This was also suggested in 1945 by Dahlberg using Butler's Field Theory that focused on evolution and development of mammalian teeth into human dentition in an attempt to analyse different of agenesis.[17] In each jaw, four morphological sites were identified (incisors, canines, premolars and molars). The tooth at the end of each region was less genetically stable and hence more prone to absence. In contrast, the tooth most mesial in each region seemed to be more genetically stable.[18] A subsequent theory hypothesised the teeth at the end of each region were possibly “vestigial bodies” that became obsolete during the evolutionary process. At present, it has been theorised that evolutionary change is working to decrease the human dentition by the loss of an incisor, premolar and molar in each quadrant. According to Vastardis (2000), the size of jaws and number of teeth seem to decrease along with human evolution.[19]
Theories focusing on anatomical principle, hypothesised that specific areas of the dental lamina are especially prone to environmental effects during tooth maturation.[16] Svinhufvud et al. (1988) suggested that teeth that were more prone to absence developed in areas of initial fusion of the jaw. For instance, maxillary lateral incisors originate where the lateral maxillae and medial nasal bone processes fuse.[20] In contrast, Kjaer et al. (1994) suggested regions where innervation developed were more sensitive than areas of fusion.[21] Commonly affected regions were found to undergo innervation last, this might imply the developmental relationship between nerve and hard tissue. It is thought to be local nerve development that affects tooth agenesis rather than global development, as brainstem anomalies have not been seen to affect tooth development.[21]
Presently, the role of polygenic and environmental factors on hypodontia is recognised in most theories.
Environmental factors
Environmental factors can be classified into 2 main groups, invasive and non-invasive. These factors act additively or independently, ultimately affecting positioning and physical development of the tooth.[22]
Invasive environmental factors potentially affect tooth development and positioning leading to hypodontia and impaction. Examples include jaw fractures, surgical procedures and extraction of the preceding deciduous tooth.[22] Treatment such as irradiation has been shown to have severe effects on developing teeth. In a smaller capacity, Chemotherapy was also found to have a similar effect. Thalidomide (N-phthaloylglutamine) was also discovered to have a causative effect on mothers who took the drug during pregnancy, resulting in congenitally missing teeth in their children. A link was found between systemic diseases, endocrine disruption (i.e. idiopathic hypoparathyroidism and pseudohypoparathyroidism).[23] and ectodermal dysplasia. However, a definite etiological relationship has yet to be established.[22] Examples of infections include rubella[24] and candida.[25] Exposure to PCBs (ex.dioxin),[26][27][28] allergy [29] and toxic epidermal necrolysis after drug.[30] may also be contributing factors.
In a recent study assessing environmental risk factors for hypodontia, it was established that maternal smoking does play a causative role in Hypodontia. Passive smoking and caffeine were also assessed but showed no statistical significance.[31]
The Journal of the American Dental Association published preliminary data suggesting a statistical association between hypodontia of the permanent teeth and epithelial ovarian cancer (EOC). The study shows that women with EOC are 8.1 times more likely to have hypodontia than are women without EOC. The suggestion therefore is that hypodontia can serve as a "marker" for potential risk of EOC in women.[32]
Genetics
Genetic causes also involve the genes MSX1 and PAX9.[33][34]
Genetic associations for selective tooth agenesis ("STHAG") include:
| Type | OMIM | Gene | Locus |
|---|---|---|---|
| STHAG1 | 106600 | MSX1 | 4p16 |
| STHAG2 | 602639 | ? | 16q12 |
| STHAG3 | 604625 | PAX9 | 14q12 |
| STHAG4 | 150400 | WNT10A | 2q35 |
| STHAG5 | 610926 | ? | 10q11 |
| STHAG6 | 613097 | LTBP3 | 11q12 |
| STHAGX1 | 313500 | EDA | Xq13.1 |
Failure of tooth formation due to disturbances during the early stages of development could be the cause of congenital missing teeth, this is also known as tooth agenesis. A variety of studies shows that missing teeth are commonly associated with genetic and environmental factors. Some literature also show that a combination of both factors may contribute to the occurrence of missing teeth.[35]
Genetics has always played a crucial role in dental aplasia. The pattern of congenitally missing teeth seen in monozygotic twins is different, suggesting an underlying epigenetic factor, which may be due to the simultaneous occurrence of two anomalies.[36] This multifactorial aetiology involves environmental factor which triggers the genetic anomalies resulting the occurrence of dental agenesis. Common environmental factors include infection, trauma and drugs which predispose to the condition. In hereditary cases, evidence of dental germ developing after surrounding tissues have closed the space required for development may be a huge contributing factor as well such as genetic disorders like down syndrome,[10] ectodermal dysplasia,[11] cleidocranial dysplasia,[37] orofacial clefting, especially cleft lip and palate.[38]
Most the craniofacial characteristics are influenced by the both genetic and environmental factors through complex interactions. The variable expressivity of traits can be either completely genetic determined, environmental determined or both. The multiplicity of hypodontia theories suggest that missing teeth are strongly influenced by genetic factor. Although single gene defect may contribute to the cause of hypodontia, but more studies propose that hypodontia is mainly the result of one or more point of genetic mutations which are closely linked, which is known as polygenic defect.[39][40][41]
Despite the aetiology of missing teeth is remained consensus, but genetic plays an important role for hypodontia is shown in many different cases.[42] There are over hundreds genes are expressed and involved in regulating tooth morphogenesis.[43][44]
MSX1
MSX1 (muscle segment homeobox 1) involved in condensation of ectomesenchyme in the tooth germ. Among the members of homeobox genes, MSX1 and MSX2 are crucial in mediating direct epithelial-mesenchymal interactions during tooth development by expressing in regions of condensing ectomesenchyme in the tooth germ.[45] MSX1 mutations have been identified as one of the contributing factors of missing second premolars, third molars, with a small percentage of first molars. MSX1 is less likely to cause anterior agenesis.[45][46][47]
Heterozygous mutations in PAX9 (paired box gene 9) could arrest tooth morphogenesis as it plays a role of transcription the gene expressed in tooth mesenchyme at the bud stage during tooth development.[48][49] A study showed that single nucleotide polymorphisms in PAX9 were highly associated with missing upper lateral incisors.[44]
AXIN2
AXIN2 (AXIS inhibition protein 2) gene is negative regulator of the Wnt signalling pathway, which is important in regulating cell fate, proliferation, differentiation and apoptosis.[50] It's polymorphic variant may be associated with hypodontia such as missing lower incisors or in a more severe form of agenesis like oligontia (lack of six or more permanent teeth).[51][52]
EDA
The EDA provides instructions for making a protein called ectodysplasin A.[53] It encodes transmembrane protein that is part of TNF (tumour necrosis factor) family of ligands. EDA gene defects cause ectodermal dysplasia, which is also known as X-linked hypohidrotic ectodermal dysplasia.[54] Common dental features of ectodermal dysplasia are multiple missing teeth and microdontia.[55]
PAX9 and TGFA are involved in regulating between MSX1 and PAX9 causing hypodontia of the molars.[36]
Hypodontia can be found in isolated cases too. The familiar or sporadic type of isolations are more frequently reported than syndromic type. Isolated cases autosomal dominant,[56][57] autosomal recessive [58][59] or X-linked [60] inheritance patterns may have an impact on the isolation conditions in expressing variation of both penetration and expressivity of traits.[61] Mutations in MSX, PAX9 and TGFA genes are known to cause congenitally missing teeth in some racial groups.
Research
In the 1960s and 1970s, several studies were conducted sponsored by the U.S. Atomic Energy Commission, with the aim of finding a link between genetics and hypodontia.[62][63]
Impacts
There is numerous studies or research report on the prevalence, aetiology,[64] treatment of hypodontia and dentoskeletal effect of hypodontia.[65] A few studies have investigated Oral Health-related Quality of Life (OHRQoL) in individuals with hypodontia[64] and provided some evidences that hypodotia may have an impact on quality of life.
Psychosocial
Cosmetic dentistry and facial aesthetic are notable for today's popular culture.[65] Interpersonal relationships and perceived qualities, for instances intelligence, friendliness, social class, and popularity from infancy to adulthood, can be affected by dentofacial appearances.[65] Some studies showed that the extent of complaints made by patients was associated with the severity of the condition and the number of missing permanent teeth.[65]
Meta-analyses and theoretical reviews demonstrated that attractive children are seen by others as more intelligent and exhibit more positive social behaviour and traits other than receiving much more positive treatment than their less attractive counterparts.[66] Therefore, a divergence from perceived ideal dentofacial aesthetic, particularly in children, might adversely affect self-esteem and self-confidence besides attracting mockery from peers.[67]
It is therefore reasonable to theorize that deviations from “normal” or “ideal” dentofacial aesthetic could be destructive to an individual's psychosocial and emotional[68] well-being, which brings upon some psychosocial distress in that individual as a result of his or her condition.[65]
Functional
Individuals with hypodontia tend to have deeper bites and spaces.[69] Further deepening of the bite can also be seen on individuals with missing posterior teeth. Apart from that, hypodontia may lead to non-working interferences, poor gingival contours and over-eruptions of the opposing teeth.[69]
It has been found that individual with hypodontia experience more difficulty during mastication or functioning movements due to smaller occlusal table available. A recent cross-sectional study showed that hypodontia patients have more difficulties in chewing, especially if the deciduous teeth associated with the missing permanent teeth had been exfoliated.[65] Despite currently limited evidence to support this statement, it is plausible that hypodontia may pose functional limitations, which eventually affect that individual's general well-being and quality of life.[69]
Financial
Patient with hypodontia requires careful treatment plan due to complex case in order to ensure the best treatment outcomes. Such treatment plans require multi-disciplinary approach, which usually come at a financial cost to both patient and possibly their family.[70] Due to this reason, a team consists of different dental specialties is involved in the patient care.[71][72]
Management
Hypodontia is a condition that can present in various ways with differing severities. This results in a wide range of treatment methods available.[73] Those affected should be allowed to consider and select the most suitable option for themselves.[74] Early diagnosis of hypodontia is critical for treatment success.[75] The treatment of hypodontia involves specialists in departments such as oral and maxillofacial surgery, operative dentistry, pediatric dentistry, orthodontics and prosthodontics.[36]
Before determining a treatment plan, the following should be determined:
- Evaluate the number of teeth missing[36][76]
- The size and number of remaining teeth in both arches[36]
- Malocclusion[36][76]
- Facial profile[36][76]
- Bone volume[36]
- Age: Definitive treatment for hypodontia only commences once all permanent teeth erupt, or upon the completion of orthodontic treatment[75][76]
- Primary teeth condition[76]
- Patient's motivation towards treatment[76]
The following below are the methods used to manage hypodontia:
Accept spacing
This is a method suitable to individuals if the space from a missing tooth is not deemed to be an aesthetic concern.[77] Spacing present behind the canines may not be particularly visible, depending on the individual.[77]
Management of retained primary teeth
When there is a case of hypodontia of the permanent premolar teeth, the primary molar teeth would often remain in situ beyond the time they are meant to exfoliate.[78] Therefore, with a presence of healthy primary teeth in the absence of a permanent successor, retaining the primary teeth can be a feasible management of hypodontia.
The primary molars present also functions as a space maintainer, prevent alveolar bone resorption and delays future prosthodontic space replacement by acting as a semi permanent solution going into adulthood[76] Previous studies also shown a good prognosis of retained primary molars going into adulthood.[79][80] However, leaving the primary teeth in place may run the risk of tooth infraocclusion i.e. submerging or progressive root resorption.[36][76]
Orthodontic space closure
Orthodontic space closure[73][81] can be an option for hypodontia management in the case of missing maxillary lateral incisors through the reshaping, and mesial re-positioning of the adjacent canine.[81] This management is indicated in hypodontia cases of Class I molar relationship with severe crowding in the mandibular anterior region where the extraction of lower premolar leads to a predictable outcome, and Class II molar relationship in the absence of crowding and protrusion of the mandibular anterior dentition.[81][82][83]
There have been several studies which showed the advantages of orthodontic space closure without prosthodontic space replacements.[82][84] The main advantage mentioned is the early completion of the treatment during early adolescence and the long lasting result of the treatment outcome. In individuals with a high smile line, the mesial re-positioning of canine maintains the normal soft tissue architecture is important in maintaining the aesthetic appearance. This option also negates the risks and costs that comes with prosthodontic treatment and the impression that there is no missing tooth.[81][82][84]
Some considerations are to be taken into account when making a decision whether to undergo space closure. These include facial profile, size and dimension of canine, the shade of colour of the teeth and the gingival contour and height.[81][82][83] Group function occlusion is usually present as a result of the mesial movement of the canine. In order to maintain the stability of the closed space, direct-bonded lingual retainers are usually required.[81]
Orthodontic space opening prior to prosthodontic treatment
The need for orthodontic space opening prior to prosthodontic management depends on the amount of edentulous space available in relation to adjacent teeth, occlusion and aesthetic concerns.[81] To determine the amount of space needed, three methods in the literature can be used which are the golden proportion, the Bolton Analysis and comparing the edentulous space with the contralateral tooth size if present.[85][86]
Space opening and prosthodontic treatment is indicated where there is a Class I molar relationships in the absence of malocclusion Class III molar relationships presenting with a concave facial profile.[81] However, the alteration in appearance during orthodontic treatment (e.g. creating diastema for placement of prostheses) before the filling up the space, although temporary, can negatively impact the oral health-related quality of life in adolescents.[87]
Removable partial dentures
Removable partial dentures are known to be an effective interim method for maintaining functional and aesthetic demands in a growing patient, where definitive fixed restorations are not suitable yet.[77] Removable dentures act as a space maintainer and also prevent the migration of adjacent or opposing teeth, thereby preserving the face height.[77] They are also easy to adjust or add on to in the event of further tooth eruption.[77] However, it may be difficult for young individuals to adhere with wearing removable dentures, due to their bulk.[77] Some patients also find the idea of dentures functionally and socially unacceptable, making them unwilling to comply.[77] Removable prosthetic devices are also known to cause damage to the remaining teeth if worn over a long period of time.[77]

Conventional crown and bridgework
Fixed restorative options are generally preferred over removable ones.[77]
- Resin-bonded bridges: Due to its minimal preparation required, this method of replacing teeth is more suited to young adults.[77] It is a definitive restoration with the ability to fill up one or two tooth spaces.[77] Research has reflected a survival rate of 80% over a period of 6 years or longer,[88] and that cantilever resin-bonded bridges are at least as good as conventional fixed-fixed bridges. Restoring teeth with this method can only be done after orthodontic treatment and will need an element of retention to ensure that tooth contacts are not misplaced.[77]
- Conventional bridges: Teeth tend to be prepared for conventional bridgework if there are large restorations present, thus being more commonly done on adult patients with hypodontia.[77] Treatment with conventional bridgework[87][75] will require significant reduction of tooth structure, which will put the tooth at risk of biological damage i.e. loss of vitality.[75] This risk is especially high in young patients with large pulp chambers.[75]
Tooth autotransplantation
Autotransplantation[74] involves the removal of a tooth from one socket and relocating to another socket in the same individual. If done successfully, it is able to ensure stable alveolar bone volume as there is continuous stimulation of the periodontal ligament.[36]
Implant supported tooth replacement
Placing dental implants has proven to be a predictable and reliable method of treating hypodontia, along with bringing excellent aesthetic results.[75] Implant placement should be delayed until jaw growth in an individual is complete.[36] One limitation of implant placement would be the need for a sufficient amount of bone volume, which if not met, may affect the positioning of the implant.[75] However, bone grafting can be carried out to overcome this.[75]
Epidemiology
Hypodontia is less common in the primary dentition [2] with reported prevalence rates ranging from 0.5% in Icelandic population [89] to 2.4% in Japanese population.[90] In the primary dentition the teeth reported as most likely to be missing are the lateral incisors, both maxillary and mandibular.[3][90] If a deciduous tooth is missing this will increase the risk of an absent successor.[91]
In the permanent dentition third molars are most commonly absent and one study [91] found prevalence rates of between 20 and 22%. When third molars are ignored the prevalence rate for each tooth varies from study to study.[2] In Caucasian studies mandibular second premolars and maxillary lateral incisors are most often absent.[2] Several UK studies have found the lower second premolar to be most commonly absent.[92][93] Studies from Asian populations report that the mandibular incisor is most commonly absent.[94]
A higher prevalence of hypodontia in females has been reported, 3:2.[93] The most extensive studies have been in Caucasian populations and suggest a prevalence of 4-6%.[92][93]
One study [95] looked at 33 previous studies with a sample size of 127000 and concluded that the prevalence of hypodontia in the permanent dentition varied between continents, racial groups and genders. In the white European population they suggested a prevalence of 4.6% in males and 6.3% in females. In an African-American sample they found this to be 3.2% in males and 4.6% in females. The same study found that in the permanent dentition the most likely teeth to be missing and the frequency of these missing teeth was:
References
- Hobkirk JA, King PA, Goodman JR, Jones SP (January 1995). "Hypodontia: 2. The management of severe hypodontia". Dental Update. 22 (1): 8–11. PMID 7664972.
- Larmour CJ, Mossey PA, Thind BS, Forgie AH, Stirrups DR (April 2005). "Hypodontia--a retrospective review of prevalence and etiology. Part I". Quintessence International. 36 (4): 263–70. PMID 15835422.
- Nandhra, S. (2013-06-14). "Hypodontia: A Team Approach to Management (2010)". The European Journal of Orthodontics. 35 (5): 717. doi:10.1093/ejo/cjt039.
- Brook AH (1984). "A unifying aetiological explanation for anomalies of human tooth number and size". Archives of Oral Biology. 29 (5): 373–8. doi:10.1016/0003-9969(84)90163-8. PMID 6611147.
- Baccetti T (June 1998). "A controlled study of associated dental anomalies". The Angle Orthodontist. 68 (3): 267–74. doi:10.1043/0003-3219(1998)068<0267:ACSOAD>2.3.CO;2 (inactive 2019-12-07). PMID 9622764.
- Brin I, Becker A, Shalhav M (February 1986). "Position of the maxillary permanent canine in relation to anomalous or missing lateral incisors: a population study". European Journal of Orthodontics. 8 (1): 12–6. doi:10.1093/ejo/8.1.12. PMID 3456897.
- Peck L, Peck S, Attia Y (1993). "Maxillary canine-first premolar transposition, associated dental anomalies and genetic basis". The Angle Orthodontist. 63 (2): 99–109, discussion 110. doi:10.1043/0003-3219(1993)063<0099:MCFPTA>2.0.CO;2 (inactive 2019-12-07). PMID 8498708.
- Al-Ani AH, Antoun JS, Thomson WM, Merriman TR, Farella M (2017). "Hypodontia: An Update on Its Etiology, Classification, and Clinical Management". BioMed Research International. 2017: 9378325. doi:10.1155/2017/9378325. PMC 5376450. PMID 28401166.
- Jiroutová O, Müllerová Z (1994). "The occurrence of hypodontia in patients with cleft lip and/or palate". Acta Chirurgiae Plasticae. 36 (2): 53–6. PMID 7618404.
- Mestrović SR, Rajić Z, Papić JS (December 1998). "Hypodontia in patients with Down's syndrome". Collegium Antropologicum. 22 Suppl: 69–72. PMID 9951143.
- "Ectodermal dysplasia and hypodontia". British Dental Journal. 212 (11): 523. June 2012. doi:10.1038/sj.bdj.2012.481.
- Rédua RB, Rédua PC (August 2018). "Hypodontia of mandibular incisors: considerations on the orthodontic treatment". Dental Press Journal of Orthodontics. 23 (4): 79–87. doi:10.1590/2177-6709.23.4.079-087.bbo. PMC 6150707. PMID 30304157.
- "Hypodontia—a Retrospective Review of Prevalence and Etiology. Part I". ResearchGate. Retrieved 2018-10-22.
- Vucic S, Dhamo B, Kuijpers MA, Jaddoe VW, Hofman A, Wolvius EB, Ongkosuwito EM (October 2016). "Craniofacial characteristics of children with mild hypodontia". American Journal of Orthodontics and Dentofacial Orthopedics. 150 (4): 611–619. doi:10.1016/j.ajodo.2016.03.021. PMID 27692418.
- {{Missing Teeth (Hypodontia and Oligodontia) - Agnès Bloch-Zupan Heddie O. Sedano Crispian Scully, Dento/Oro/Craniofacial Anomalies and Genetics, 2012, Pages 9–74]]
- Galluccio G, Castellano M, La Monaca C (July 2012). "Genetic basis of non-syndromic anomalies of human tooth number". Archives of Oral Biology. 57 (7): 918–30. doi:10.1016/j.archoralbio.2012.01.005. PMID 22325622.
- Husam, Al-Ani, Azza (2016). Genetic and environmental factors associated with hypodontia (Thesis). University of Otago. hdl:10523/6866.
- Hobkirk JA, Goodman JR, Jones SP (November 1994). "Presenting complaints and findings in a group of patients attending a hypodontia clinic". British Dental Journal. 177 (9): 337–9. doi:10.1038/sj.bdj.4808606. PMID 7980981.
- Vastardis H (June 2000). "The genetics of human tooth agenesis: new discoveries for understanding dental anomalies". American Journal of Orthodontics and Dentofacial Orthopedics. 117 (6): 650–6. doi:10.1016/s0889-5406(00)70173-9. PMID 10842107.
- Svinhufvud E, Myllärniemi S, Norio R (December 1988). "Dominant inheritance of tooth malpositions and their association to hypodontia". Clinical Genetics. 34 (6): 373–81. doi:10.1111/j.1399-0004.1988.tb02895.x. PMID 3233785.
- Kjaer I, Kocsis G, Nodal M, Christensen LR (October 1994). "Aetiological aspects of mandibular tooth agenesis--focusing on the role of nerve, oral mucosa, and supporting tissues". European Journal of Orthodontics. 16 (5): 371–5. doi:10.1093/ejo/16.5.371. PMID 7805810.
- J Pemberton T, Das P, Patel P (2004-11-30). "Hypodontia: Genetics and future perspectives". Brazilian Journal of Oral Sciences. 4 (13).
- Sutphin A, Albright F, McCune DJ (1943). "Five cases (3 in siblings) of idiopathic hypoparathyroidism associated with moniliasis". J. Clin. Endocrinol. 3 (12): 625–634. doi:10.1210/jcem-3-12-625.
- Wu CC, Wong RW, Hägg U (2007). "A review of hypodontia: the possible etiologies and orthodontic, surgical and restorative treatment options—conventional and futuristic" (PDF). Hong Kong Dental Journal. 4: 113–21.
- Kinirons MJ (June 1983). "Candidal invasion of dentine complicating hypodontia". British Dental Journal. 154 (12): 400–1. doi:10.1038/sj.bdj.4805102. PMID 6576802.
- Alaluusua S, Lukinmaa PL, Torppa J, Tuomisto J, Vartiainen T (January 1999). "Developing teeth as biomarker of dioxin exposure". Lancet. 353 (9148): 206. doi:10.1016/S0140-6736(05)77214-7. PMID 9923879.
- Alaluusua S, Calderara P, Gerthoux PM, Lukinmaa PL, Kovero O, Needham L, Patterson DG, Tuomisto J, Mocarelli P (September 2004). "Developmental dental aberrations after the dioxin accident in Seveso". Environmental Health Perspectives. 112 (13): 1313–8. doi:10.1289/ehp.6920. PMC 1247522. PMID 15345345.
- Guo YL, Lambert GH, Hsu CC, Hsu MM (April 2004). "Yucheng: health effects of prenatal exposure to polychlorinated biphenyls and dibenzofurans". International Archives of Occupational and Environmental Health. 77 (3): 153–8. doi:10.1007/s00420-003-0487-9. PMID 14963712.
- Yamaguchi T, Tomoyasu Y, Nakadate T, Oguchi K, Maki K (December 2008). "Allergy as a possible predisposing factor for hypodontia". European Journal of Orthodontics. 30 (6): 641–4. doi:10.1093/ejo/cjn043. PMID 18687988.
- Gaultier F, Rochefort J, Landru MM, Allanore L, Naveau A, Roujeau JC, Gogly B (November 2009). "Severe and unrecognized dental abnormalities after drug-induced epidermal necrolysis". Archives of Dermatology. 145 (11): 1332–3. doi:10.1001/archdermatol.2009.233. PMID 19917972.
- Al-Ani AH, Antoun JS, Thomson WM (August 2017). "Maternal Smoking During Pregnancy is associated with Offspring Hypodontia". J Dent Res. 96 (9): 1014–1019. doi:10.1177/0022034517711156. PMID 28535361.
- Chalothorn LA, Beeman CS, Ebersole JL, Kluemper GT, Hicks EP, Kryscio RJ, DeSimone CP, Modesitt SC (February 2008). "Hypodontia as a risk marker for epithelial ovarian cancer: a case-controlled study". Journal of the American Dental Association. 139 (2): 163–9. doi:10.14219/jada.archive.2008.0132. PMID 18245684.
- Nieminen P (June 2009). "Genetic basis of tooth agenesis". Journal of Experimental Zoology Part B: Molecular and Developmental Evolution. 312B (4): 320–42. doi:10.1002/jez.b.21277. PMID 19219933.
- De Coster PJ, Marks LA, Martens LC, Huysseune A (January 2009). "Dental agenesis: genetic and clinical perspectives". Journal of Oral Pathology & Medicine. 38 (1): 1–17. doi:10.1111/j.1600-0714.2008.00699.x. PMID 18771513.
- Harris EF (June 2008). "Interpreting heritability estimates in the orthodontic literature". Seminars in Orthodontics. 14 (2): 125–134. doi:10.1053/j.sodo.2008.02.003.
- Rakhshan V (2015). "Congenitally missing teeth (hypodontia): A review of the literature concerning the etiology, prevalence, risk factors, patterns and treatment". Dental Research Journal. 12 (1): 1–13. doi:10.4103/1735-3327.150286. PMC 4336964. PMID 25709668.
- Chopra R, Marwaha M, Chaudhuri P, Bansal K, Chopra S (2012). "Hypodontia and delayed dentition as the primary manifestation of cleidocranial dysplasia presenting with a diagnostic dilemma". Case Reports in Dentistry. 2012: 262043. doi:10.1155/2012/262043. PMC 3540686. PMID 23320199.
- Slayton RL, Williams L, Murray JC, Wheeler JJ, Lidral AC, Nishimura CJ (May 2003). "Genetic association studies of cleft lip and/or palate with hypodontia outside the cleft region". The Cleft Palate-Craniofacial Journal. 40 (3): 274–9. doi:10.1597/1545-1569_2003_040_0274_gasocl_2.0.co_2. PMC 2752356. PMID 12733956.
- Vastardis H (June 2000). "The genetics of human tooth agenesis: new discoveries for understanding dental anomalies". American Journal of Orthodontics and Dentofacial Orthopedics. 117 (6): 650–6. doi:10.1016/S0889-5406(00)70173-9. PMID 10842107.
- "Hypodontia—a Retrospective Review of Prevalence and Etiology. Part I". ResearchGate. Retrieved 2018-10-22.
- Brook AH (1984-01-01). "A unifying aetiological explanation for anomalies of human tooth number and size". Archives of Oral Biology. 29 (5): 373–8. doi:10.1016/0003-9969(84)90163-8. PMID 6611147.
- Bäckman B, Wahlin YB (January 2001). "Variations in number and morphology of permanent teeth in 7-year-old Swedish children". International Journal of Paediatric Dentistry. 11 (1): 11–7. doi:10.1046/j.1365-263x.2001.00205.x. PMID 11309867.
- Kapadia H, Mues G, D'Souza R (August 2007). "Genes affecting tooth morphogenesis". Orthodontics & Craniofacial Research. 10 (3): 105–13. doi:10.1111/j.1601-6343.2007.00395.x. PMID 17651126.
- Alves-Ferreira M, Pinho T, Sousa A, Sequeiros J, Lemos C, Alonso I (May 2014). "Identification of genetic risk factors for maxillary lateral incisor agenesis". Journal of Dental Research. 93 (5): 452–8. doi:10.1177/0022034514523986. PMID 24554542.
- MacKenzie A, Ferguson MW, Sharpe PT (June 1992). "Expression patterns of the homeobox gene, Hox-8, in the mouse embryo suggest a role in specifying tooth initiation and shape". Development. 115 (2): 403–20. PMID 1358591.
- Gökkaya B, Motro M, Kargül B (2015). "Prevalence and characteristics of non-syndromic hypodontia among Turkish orthodontic patient population". Journal of International Society of Preventive & Community Dentistry. 5 (3): 170–5. doi:10.4103/2231-0762.159952. PMC 4515798. PMID 26236675.
- Vastardis H, Karimbux N, Guthua SW, Seidman JG, Seidman CE (August 1996). "A human MSX1 homeodomain missense mutation causes selective tooth agenesis". Nature Genetics. 13 (4): 417–21. doi:10.1038/ng0896-417. PMID 8696335.
- Mitsui SN, Yasue A, Masuda K, Watanabe K, Horiuchi S, Imoto I, Tanaka E (March 2014). "Novel PAX9 mutations cause non-syndromic tooth agenesis". Journal of Dental Research. 93 (3): 245–9. doi:10.1177/0022034513519801. PMID 24436340.
- Cobourne MT, Sharpe PT (2012-05-25). "Diseases of the tooth: the genetic and molecular basis of inherited anomalies affecting the dentition". Wiley Interdisciplinary Reviews: Developmental Biology. 2 (2): 183–212. doi:10.1002/wdev.66. PMID 24009033.
- Callahan N, Modesto A, Meira R, Seymen F, Patir A, Vieira AR (January 2009). "Axis inhibition protein 2 (AXIN2) polymorphisms and tooth agenesis". Archives of Oral Biology. 54 (1): 45–9. doi:10.1016/j.archoralbio.2008.08.002. PMC 2643013. PMID 18790474.
- Lammi L, Arte S, Somer M, Jarvinen H, Lahermo P, Thesleff I, Pirinen S, Nieminen P (May 2004). "Mutations in AXIN2 cause familial tooth agenesis and predispose to colorectal cancer". American Journal of Human Genetics. 74 (5): 1043–50. doi:10.1086/386293. PMC 1181967. PMID 15042511.
- Mostowska A, Biedziak B, Jagodzinski PP (2006-01-24). "Axis inhibition protein 2 (AXIN2) polymorphisms may be a risk factor for selective tooth agenesis". Journal of Human Genetics. 51 (3): 262–6. doi:10.1007/s10038-005-0353-6. PMID 16432638.
- "EDA ectodysplasin A [Homo sapiens (human)] - Gene - NCBI". www.ncbi.nlm.nih.gov. Retrieved 2018-10-22.
- Kere J, Srivastava AK, Montonen O, Zonana J, Thomas N, Ferguson B, Munoz F, Morgan D, Clarke A, Baybayan P, Chen EY, Ezer S, Saarialho-Kere U, de la Chapelle A, Schlessinger D (August 1996). "X-linked anhidrotic (hypohidrotic) ectodermal dysplasia is caused by mutation in a novel transmembrane protein". Nature Genetics. 13 (4): 409–16. doi:10.1038/ng0895-409. PMID 8696334.
- "A Dentist Recognizes Ectodermal Dysplasia and Brings Welcome Relief to Family | jcda". www.jcda.ca. Retrieved 2018-10-22.
- Arte S, Nieminen P, Apajalahti S, Haavikko K, Thesleff I, Pirinen S (May 2001). "Characteristics of incisor-premolar hypodontia in families". Journal of Dental Research. 80 (5): 1445–50. doi:10.1177/00220345010800051201. PMID 11437217.
- Goldenberg M, Das P, Messersmith M, Stockton DW, Patel PI, D'Souza RN (July 2000). "Clinical, radiographic, and genetic evaluation of a novel form of autosomal-dominant oligodontia". Journal of Dental Research. 79 (7): 1469–75. doi:10.1177/00220345000790070701. PMID 11005730.
- Pirinen S, Kentala A, Nieminen P, Varilo T, Thesleff I, Arte S (August 2001). "Recessively inherited lower incisor hypodontia". Journal of Medical Genetics. 38 (8): 551–6. doi:10.1136/jmg.38.8.551. PMC 1734917. PMID 11494968.
- Ahmad W, Brancolini V, ul Faiyaz MF, Lam H, ul Haque S, Haider M, Maimon A, Aita VM, Owen J, Brown D, Zegarelli DJ, Ahmad M, Ott J, Christiano AM (April 1998). "A locus for autosomal recessive hypodontia with associated dental anomalies maps to chromosome 16q12.1". American Journal of Human Genetics. 62 (4): 987–91. doi:10.1086/301799. PMC 1377039. PMID 9529357.
- Han D, Gong Y, Wu H, Zhang X, Yan M, Wang X, Qu H, Feng H, Song S (November 2008). "Novel EDA mutation resulting in X-linked non-syndromic hypodontia and the pattern of EDA-associated isolated tooth agenesis". European Journal of Medical Genetics. 51 (6): 536–46. doi:10.1016/j.ejmg.2008.06.002. PMID 18657636.
- Graber LW (February 1978). "Congenital absence of teeth: a review with emphasis on inheritance patterns". Journal of the American Dental Association. 96 (2): 266–75. doi:10.14219/jada.archive.1978.0054. PMID 342579.
- Niswander JD, Sujaku C (December 1963). "Congenital anomalies of teeth in Japanese children". American Journal of Physical Anthropology. 21 (4): 569–74. doi:10.1002/ajpa.1330210413. PMID 14185534.
- Woolf CM (May 1971). "Missing maxillary lateral incisors: a genetic study". American Journal of Human Genetics. 23 (3): 289–96. PMC 1706719. PMID 5089845.
- Meaney, S.; Anweigi, L.; Ziada, H.; Allen, F. (2011-06-21). "The impact of hypodontia: a qualitative study on the experiences of patients". The European Journal of Orthodontics. 34 (5): 547–552. doi:10.1093/ejo/cjr061. ISSN 0141-5387. PMID 21693681.
- Emma, Laing (Jan 2010). "Psychosocial impact of hypodontia in children". American Journal of Orthodontics and Dentofacial Orthopedics. 137.
- "PsycNET". psycnet.apa.org. Retrieved 2018-11-26.
- Shaw, W C; O'Brien, K D; Richmond, S; Brook, P (1991). "Quality control in orthodontics: risk/benefit considerations". British Dental Journal. 170 (1): 33–37. doi:10.1038/sj.bdj.4807399. ISSN 0007-0610. PMID 2001299.
- SHEENA, KOTECHA. "The Impact of Hypodontia on the Oral Health Related-Quality of Life in Children" (PDF).
- Al-Ani, Azza Husam; Antoun, Joseph Safwat; Thomson, William Murray; Merriman, Tony Raymond; Farella, Mauro (2017). "Hypodontia: An Update on Its Etiology, Classification, and Clinical Management". BioMed Research International. 2017: 9378325. doi:10.1155/2017/9378325. ISSN 2314-6133. PMC 5376450. PMID 28401166.
- J. A., Hobkirk; D., Gill; S. P., Jones (2011). Hypodontia A Team Approach to Management. ISBN 978-1-405-18859-3.
- Parkin, N.; Elcock, C.; Smith, R.N.; Griffin, R.C.; Brook, A.H. (2009-12-01). "The aetiology of hypodontia: The prevalence, severity and location of hypodontia within families". Archives of Oral Biology. 54: S52–S56. doi:10.1016/j.archoralbio.2008.11.002. ISSN 0003-9969. PMID 19100963.
- SCHALK-VAN DER WEIDE, Y.; STEEN, W.H.A.; BOSMAN, F. (1993). "Taurodontism and length of teeth in patients with oligodontia". Journal of Oral Rehabilitation. 20 (4): 401–412. doi:10.1111/j.1365-2842.1993.tb01624.x. ISSN 0305-182X. PMID 8350175.
- Barber S, Bekker HL, Meads D, Pavitt S, Khambay B (February 2018). "Identification and appraisal of outcome measures used to evaluate hypodontia care: A systematic review" (PDF). American Journal of Orthodontics and Dentofacial Orthopedics. 153 (2): 184–194.e18. doi:10.1016/j.ajodo.2017.10.010. PMID 29407495.
- Barber S, Bekker HL, Meads D, Pavitt S, Khambay B (February 2018). "Identification and appraisal of outcome measures used to evaluate hypodontia care: A systematic review" (PDF). American Journal of Orthodontics and Dentofacial Orthopedics. 153 (2): 184–194.e18. doi:10.1016/j.ajodo.2017.10.010. PMID 29407495.
- Valle AL, Lorenzoni FC, Martins LM, Valle CV, Henriques JF, Almeida AL, Pegoraro LF (October 2011). "A multidisciplinary approach for the management of hypodontia: case report". Journal of Applied Oral Science. 19 (5): 544–8. doi:10.1590/S1678-77572011000500018. PMC 3984204. PMID 21986661.
- Hvaring CL, Øgaard B, Stenvik A, Birkeland K (February 2014). "The prognosis of retained primary molars without successors: infraocclusion, root resorption and restorations in 111 patients". European Journal of Orthodontics. 36 (1): 26–30. doi:10.1093/ejo/cjs105. PMID 23314329.
- Jepson NJ, Nohl FS, Carter NE, Gillgrass TJ, Meechan JG, Hobson RS, Nunn JH (March 2003). "The interdisciplinary management of hypodontia: restorative dentistry". British Dental Journal. 194 (6): 299–304. doi:10.1038/sj.bdj.4809940. PMID 12682653.
- Sletten DW, Smith BM, Southard KA, Casko JS, Southard TE (December 2003). "Retained deciduous mandibular molars in adults: a radiographic study of long-term changes". American Journal of Orthodontics and Dentofacial Orthopedics. 124 (6): 625–30. doi:10.1016/j.ajodo.2003.07.002. PMID 14666074.
- Bjerklin K, Al-Najjar M, Kårestedt H, Andrén A (June 2008). "Agenesis of mandibular second premolars with retained primary molars: a longitudinal radiographic study of 99 subjects from 12 years of age to adulthood". European Journal of Orthodontics. 30 (3): 254–61. doi:10.1093/ejo/cjn027. PMID 18540014.
- Ith-Hansen K, Kjaer I (June 2000). "Persistence of deciduous molars in subjects with agenesis of the second premolars". European Journal of Orthodontics. 22 (3): 239–43. doi:10.1093/ejo/22.3.239. PMID 10920556.
- Kiliaridis S, Sidira M, Kirmanidou Y, Michalakis K (2016). "Treatment options for congenitally missing lateral incisors". European Journal of Oral Implantology. 9 Suppl 1: S5–24. PMID 27314109.
- Rosa M, Zachrisson BU (April 2001). "Integrating esthetic dentistry and space closure in patients with missing maxillary lateral incisors". Journal of Clinical Orthodontics. 35 (4): 221–34. PMID 11345569.
- Kokich VO, Kinzer GA (2005). "Managing congenitally missing lateral incisors. Part I: Canine substitution". Journal of Esthetic and Restorative Dentistry. 17 (1): 5–10. doi:10.1111/j.1708-8240.2005.tb00076.x. PMID 15934680.
- Zachrisson BU, Rosa M, Toreskog S (April 2011). "Congenitally missing maxillary lateral incisors: canine substitution. Point". American Journal of Orthodontics and Dentofacial Orthopedics. 139 (4): 434–444. doi:10.1016/j.ajodo.2011.02.003. PMID 21457853.
- Kinzer GA, Kokich VO (2005). "Managing congenitally missing lateral incisors. Part II: tooth-supported restorations". Journal of Esthetic and Restorative Dentistry. 17 (2): 76–84. doi:10.1111/j.1708-8240.2005.tb00089.x. PMID 16036123.
- Kinzer GA, Kokich VO (2005). "Managing congenitally missing lateral incisors. Part III: single-tooth implants". Journal of Esthetic and Restorative Dentistry. 17 (4): 202–10. doi:10.1111/j.1708-8240.2005.tb00116.x. PMID 16231491.
- Filius MA, Cune MS, Raghoebar GM, Vissink A, Visser A (May 2016). "Prosthetic treatment outcome in patients with severe hypodontia: a systematic review". Journal of Oral Rehabilitation. 43 (5): 373–87. doi:10.1111/joor.12384. PMID 26899287.
- Creugers NH, Käyser AF, Van't Hof MA (November 1992). "A seven-and-a-half-year survival study of resin-bonded bridges". Journal of Dental Research. 71 (11): 1822–5. doi:10.1177/00220345920710111101. PMID 1401445.
- Magnússon, T. E. (June 1984). "Hypodontia, hyperodontia, and double formation of primary teeth in Iceland. An epidemiological study". Acta Odontologica Scandinavica. 42 (3): 137–139. doi:10.3109/00016358408993864. ISSN 0001-6357. PMID 6332449.
- Stirrups, David. "Hypodontia: A retrospective review of prevalence and etiology. Part I". Quintessence International.
- Sisman, Yildiray; Uysal, Tancan; Gelgor, Ibrahim Erhan (July 2007). "Hypodontia. Does the Prevalence and Distribution Pattern Differ in Orthodontic Patients?". European Journal of Dentistry. 1 (3): 167–173. doi:10.1055/s-0039-1698333. ISSN 1305-7456. PMC 2638243. PMID 19212561.
- Sheikhi, Mahnaz; Sadeghi, Mohammad Ali; Ghorbanizadeh, Sajad (December 2012). "Prevalence of congenitally missing permanent teeth in Iran". Dental Research Journal. 9 (Suppl 1): 105–111. ISSN 1735-3327. PMC 3692187. PMID 23814548.
- Mukhopadhyay, Santanu; Mitra, Sanjib (2014). "Anomalies in primary dentition: Their distribution and correlation with permanent dentition". Journal of Natural Science, Biology, and Medicine. 5 (1): 139–143. doi:10.4103/0976-9668.127313. ISSN 0976-9668. PMC 3961919. PMID 24678213.
- "Hypodontia—a Retrospective Review of Prevalence and Etiology. Part I". ResearchGate. Retrieved 2018-10-28.
- Polder, Bart J.; Van't Hof, Martin A.; Van der Linden, Frans P. G. M.; Kuijpers-Jagtman, Anne M. (June 2004). "A meta-analysis of the prevalence of dental agenesis of permanent teeth". Community Dentistry and Oral Epidemiology. 32 (3): 217–226. doi:10.1111/j.1600-0528.2004.00158.x. ISSN 0301-5661. PMID 15151692.