We need you! Join our contributor community and become a WikEM editor through our open and transparent promotion process.
Head trauma (main)
From WikEM
(Redirected from Traumatic brain injury)
Contents
Background
- Main goals in management:
- Prevent intracranial hypertension
- Prevent secondary brain insults
- Maintain CPP > 70 mmHg
- Optimize cerebral oxygenation and blood flow
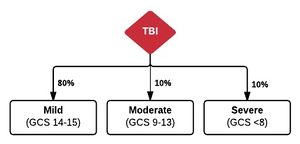
- Severe TBI defined as head trauma and GCS 3-8[1]
Clinical Features
Adult GCS
| Eye Opening | Verbal | Motor |
| 6: Obeys commands | ||
| 5: Oriented | 5: Localizes to pain | |
| 4: Spontaneously opens | 4: Confused speech | 4: Withdraws from pain (normal flexion) |
| 3: Opens to command | 3:Inappropriate words | 3: Decorticate posturing (abnormal flexion) |
| 2: Opens to pain | 2: Incomprehensible sounds | 2: Decerebrate posturing (extension) |
| 1: Does not open | 1: No response | 1: No response |
- 14-15: Mild
- 9-13: Moderate
- 3-8: Severe
Differential Diagnosis
Intracranial Hemorrhage
- Intra-axial
- Hemorrhagic stroke (Spontaneous intracerebral hemorrhage)
- Traumatic intracerebral hemorrhage
- Extra-axial
- Epidural hemorrhage
- Subdural hemorrhage
- Subarachnoid hemorrhage (aneurysmal intracranial hemorrhage)
Maxillofacial Trauma
- Le Fort fractures
- Skull fracture (peds)
- Auricular hematoma
- Nasal fracture
- Zygomatic arch fracture
- Zygomaticomaxillary (tripod) fracture
- Dental trauma
- Mandible fracture
Orbital trauma
Acute
- Ruptured Globe^
- Corneal Abrasion
- Ocular foreign body
- Conjunctival laceration
- Caustic Keratoconjunctivitis^^
- Subconjunctival hemorrhage
- Traumatic iritis
- Traumatic hyphema
- Retinal detachment
- Retrobulbar hemorrhage/hematoma
- Traumatic mydriasis
- Orbital fracture
- Frontal sinus fracture
- Naso-ethmoid fracture
- Inferior orbial wall fracture
- Medial orbital wall fracture
Subacute/Delayed
Blunt Neck Trauma
- Spinal cord trauma
- Vertebral and carotid artery dissection
- Whiplash injury
- Cervical spine fractures and dislocations
- Strangulation
Other
Evaluation
- Consider brain CT (rule out intracranial hemorrhage)
- Use validated decision rule to determine need
- Avoid CT in patients with minor head injury who are at low risk based on validated decision rules.[2]
- Consider cervical and/or facial CT
- Pertinent labs
- Blood glucose
- Venous blood
- Hemoglobin assessment with consideration for transfusion with Hb < 7 mg/dL
- PT/INR/PTT
- Electrolytes
- Hyponatremia, hypomagnesemia, and hypophosphatemia may lower the seizure threshold
- Miscellaneous labs
- Beta-2 transferrin for CSF leak, needs 0.5 cc of fluid[3]
Monitoring
- Core temperature, Foley with bladder probe
- ICP monitoring
- Jugular venous oxygen saturation (SjvO2) by retrograde catherization of right IVJ associated with improved outcomes[4]
- Normal range 55-70%
- Sustained desaturation < 50% requires aggressive treatment[5]
- Transcranial doppler around thinner walls of skull (insonation windows)[6][7]
- Temporal region above zygomatic arch, through eyes, below jaw, behind occiput
- Sensitivity for brain death is ~75%, specificity 98%
Management
- Monitor for increased ICP
- Monitor for herniation
- Maintain PaO2 > 60 mmHg
- Prevent hyperthermia
- Prevent hypotension
- Correct coagulopathy (FFP, vitamin K, PCC, desmopressin)
- Tranexemic acid may reduce progressive ICH[8]
- Loading dose 1 g over 10 min
- Followed by maintenance dose of 1 g over 8 hrs
Increased ICP Treatment[9]
Head of Bed elevation
- 30 degrees or reverse Trendelenburg will lower ICP[10]
- Keep head and neck in neutral position, improving cerebral venous drainage
- Avoid compressing IVJ or EVJ with tight C-collars or fixation of ETT
Maintain cerebral perfusion
- CPP = MAP-ICP
- If MAP <80, then CPP<60
- Ultimately no Class 1 evidence for optimal CPP
- Transfuse PRBCs with goal Hb > 10 mg/dL in severe TBI[11]
- Provide fluids and vasopressors if needed for goal cerebral perfusion pressure (CPP) of 70-80 mmHg[12][13][14]
- Mortality increases 20% for each 10 mmHg loss of CPP
- Avoid dips in CPP < 70 mmHg, which is associated with cerebral ischemia and glutamate increase[15]
- Vasopressors
- Phenylephrine increases CPP without increasing ICP in animal models[16][17]
- May be beneficial when patient is tachycardic (reflex bradycardia), but avoid phenylephrine if patient is already bradycardic (Cushing's reflex)
- Phenylephrine may be associated with less cell injury as compared to norepinephrine in TBI[18]
- IV fluids[19]
- Maintain euvolemia, initially resuscitate with Normal Saline
- Then consider hypertonic saline and/or mannitol
- Do not use free water, low osmolal, dextrose-alone solutions, and colloids
- Do not use Ringer's lactate as it is slightly hypotonic
- Prefer NS over D5-NS if possible, but D5-NS may be necessary to avoid hypoglycemia, especially in younger pediatric patients
- Correction of severe hypernatremia > 160 mmol/L (hypothalamic-pituitary injury, diabetes insipidus) should be gradual to not worsen cerebral edema
Osmotherapies
Therapies include either mannitol or hypertonic saline. In choosing the appropriate agent, coordinate with neurosurgery and take into account the patient's blood pressure. Mannitol may cause hypotension due to the osmotic diuresis.
- Mannitol[20]
- If SBP > 90 mmHg
- Bolus 20% at 0.25-1 gm/kg as rapid infusion over 15-20 min
- Target Osm 300-320 mOsm/kg
- Reduces ICP within 30min, duration of action of 6-8hr
- Monitor I/O to maintain euvolemia during expected diuresis and use normal saline to volume replace
- Do not use continuous infusions, as mannitol crosses the BBB after prolonged administration and contributes to cerebral edema
- Consider hypertonic saline for further boluses
- Hypertonic saline has higher osmotic gradient and is less permeable across BBB than mannitol
- Hypertonic saline may be more effective than mannitol, current standard of care[21]
- Obtain baseline serum osmolarity and sodium
- Most studies used 250 mL bolus of 7.5% saline with dextran[22]
- Initial 250 cc bolus of 3% will reduce ICP and can be delivered through a peripheral line
- Target sodium 145-155 mmol/dL
Prevent Cerebral Vasoconstriction
- Hyperventilation does not improve mortality, used only as temporizing measure
- Should only be used if reduction in ICP necessary without any other means or ICP elevation refractory to all other treatments:
- Sedation
- Paralytics
- CSF drainage
- Hypertonic saline, osmotic diuretics
- Maintain PaCO2 35-40 mmHg for only up to 30 minutes, no longer if it can be avoided[23]
- Hyperventilation to PaCO2 < 30 mmHg not indicated, and decreases cerebral blood flow to ischemic levels[24][25]
Seizure Control
- Treat immediately with benzodiazepines and antiepileptic drugs (AEDs)
- Consider propofol for post-intubation sedation
- Seizure prophylaxis reduces seizures but does not improve long-term outcomes[26]
- AEDs prevent early seizures (which occur between 24 hrs - 7 days), with NNT = 10 by Cochrane Review[27]
- Risk factors for post-traumatic seizures:
- GCS < 10 initially
- Cortical contusion
- Depressed skull fx
- Subdural hematoma, epidural hematoma
- Subarachnoid hemorrhage or ICH
- Penetrating head injury
- Seizure within 24 hours of injury (immediate seizure)
- Treat any clinically apparent and EEG confirmed seizures
- Consider prophylaxis in patients with any risk factors as above
- Phenytoin or fosphenytoin first line agent by BTF guidelines[28]
- Load 20 PE/kg IV, then 100 PE IV q8hrs for 7 days
- Measure serum levels to titrate to therapeutic levels
- Levetiracetam may be used as alternative[29]
- 20 mg/kg load IV, followed by 1000 mg IV q12h for 7 days
- Levetiracetam may have less frequent and severe adverse drug side effects events as compared to phenytoin
Intubation Pretreatment
Goal cerebral perfusion pressure (CPP) ~70mmHg
- If need for RSI, consider pretreatment with lidocaine and/or fentanyl
- Also ensure adequate sedation (prevent gag reflex)
- Etomidate may cause adrenal insufficiency especially in head injured patients, so consider hydrocortisone if refractory hypotension post-intubation[30]
Decrease metabolic rate
- Provide adequate sedation and analgesia
- Avoid HYPERthermia and treat fever aggressively
- However, hypothermia is not a necessary goal
- Moderate hypothermia 32°C to 34°C controversial, large RCT showed no effect[31]
Other Critical Care Measures
- DVT prophylaxis with SCDs, no anticoagulation
- Stress ulcer prophylaxis with H2-blocker/PPI and sucralfate to avoid Cushing's ulcers
- Good glycemic control, but tight maintenance not supported[32]
- Steroids, methylprednisolone contraindicated in severe TBI (risk of death increased in CRASH 2004 trial)[33]
- Routine paralysis not indicated[34]
- Increased risk of pneumonia and ICU length of stay
- However, may be used for refractory ICP elevation
Barbituate Coma[35]
- For ICP refractory to maximal medical and surgical therapy
- Only for hemodynamically stable patients
- Induce with the following:
- Pentobarbital 10 mg/kg over 30 min
- Then 5 mg/kg/hr for 3 hrs
- Followed by 1 mg/kg/hr
See Also
References
- ↑ Teasdale G, Jennett B: Assessment of coma and impaired consciousness: A practical scale. Lancet. 1974, 2: 81-84.
- ↑ Choosing wisely ACEP
- ↑ Arup Laboratories. https://arupconsult.com/content/cerebrospinal-fluid-csf-leak-beta-2-transferrin.
- ↑ Cruz J: The first decade of continuous monitoring of jugular bulb oxyhemoglobin saturation: management strategies and clinical outcome. Crit Care Med. 1998, 26: 344-351.
- ↑ Robertson CS, Cormio M: Cerebral metabolic management. New Horiz. 1995, 3: 410-422.
- ↑ de Freitas GR, Andre C: Sensitivity of transcranial Doppler for confirming brain death: A prospective study of 270 cases. Acta Neurol Scand. 2006, 113: 426-432.
- ↑ Dosemeci L, Dora B, Yilmaz M, et al: Utility of transcranial Doppler ultrasonography for confirmatory diagnosis of brain death: Two sides of the coin. Transplantation. 2004, 77: 71-75.
- ↑ Yutthakasemsunt S et al. Tranexamic Acid for Patients With Traumatic Brain Injury. BMC Emerg Med. 2013;13.
- ↑ Brain Trauma Foundation, American Association of Neurological Surgeons, Congress of Neurological Surgeons. Guidelines for the management of severe traumatic brain injury. J Neurotrauma. 2007;24 Suppl 1(supplement 1):S1-S106.fulltext
- ↑ Schwarz S et al. Effects of body position on intracranial pressure and cerebral perfusion in patients with large hemispheric stroke. Stroke. 2002; 33: 497-501
- ↑ Schöchl H, Solomon C, Traintinger S, Nienaber U, Tacacs-Tolnai A, Windhofer C, Bahrami S, Voelckel W: Thromboelastometric (ROTEM) findings in patients suffering from isolated severe traumatic brain injury. J Neurotrauma. 2011, 28 (10): 2033-2041.
- ↑ Bouma GJ et al. Blood pressure and intracranial pressure-volume dynamics in severe head injury: relationship with cerebral blood flow. J Neurosurg 77:15-19, 1992
- ↑ Rosner MJ et al. Cerebral perfusion pressure management in head injury. J Trauma 30:933-941, 1990
- ↑ Kirkman MA, Smith M. Intracranial pressure monitoring, cerebral perfusion pressure estimation, and ICP/CPP-guided therapy: a standard of care or optional extra after brain injury? Br J Anaesth. 2014 Jan;112(1):35-46.
- ↑ Vespa P. What is the Optimal Threshold for Cerebral Perfusion Pressure Following Traumatic Brain Injury? Neurosurg Focus. 2003;15(6).
- ↑ Friess SH et al. Early cerebral perfusion pressure augmentation with phenylephrine after traumatic brain injury may be neuroprotective in a pediatric swine model. Crit Care Med. 2012 Aug;40(8):2400-6.
- ↑ Watts AD et al. Phenylephrine increases cerebral perfusion pressure without increasing intracranial pressure in rabbits with balloon-elevated intracranial pressure. J Neurosurg Anesthesiol. 2002 Jan;14(1):31-4.
- ↑ Friess SH et al. Differing Effects when Using Phenylephrine and Norepinephrine To Augment Cerebral Blood Flow after Traumatic Brain Injury in the Immature Brain. J Neurotrauma. 2015 Feb 15; 32(4): 237–243.
- ↑ Haddad SH and Arabi YM. Critical care management of severe traumatic brain injury in adults. Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine201220:12.
- ↑ Muizelaar JP, Lutz HA, Becker DP: Effect of mannitol on ICP and CBF and correlation with pressure autoregulation in severely head-injured patients. J Neurosurg. 1984, 61: 700-706.
- ↑ Kamel H, Navi BB, Nakagawa K, Hemphill JC, Ko NU: Hypertonic saline versus mannitol for the treatment of elevated intracranial pressure: a meta-analysis of randomized clinical trials. Crit Care Med. 2011, 39 (3): 554-559.
- ↑ Holmes, J. Therapeutic uses of Hypertonic Saline in the Critically Ill Emergency Department Patient. EB Medicine 2013
- ↑ Coles JP, Minhas PS, Fryer TD, Smielewski P, Aigbirihio F, Donovan T, Downey SP, Williams G, Chatfield D, Matthews JC, Gupta AK, Carpenter TA, Clark JC, Pickard JD, Menon DK: Effect of hyperventilation on cerebral blood flow in traumatic head injury: clinical relevance and monitoring correlates. Crit Care Med. 2002, 30 (9): 1950-1959.
- ↑ Stocchetti N et al. Hyperventilation in head injury: a review. Chest. 2005 May;127(5):1812-27.
- ↑ Bullock R, et al: Guidelines for the Management of Severe Traumatic Brain Injury. J Neurotrauma. 2007, 24 (Suppl 1): S1-S106.
- ↑ Khan AA, Banerjee A. The role of prophylactic anticonvulsants in moderate to severe head injury. Int J Emerg Med. 2010 Jul 22;3(3):187-91.
- ↑ Thompson K, Pohlmann-Eden B, Campbell LA. Pharmacological treatments for preventing epilepsy following traumatic head injury (Protocol). Cochrane Database of Systematic Reviews 2012, Issue 6. Art. No.: CD009900.
- ↑ Khan AA, Banerjee A. The role of prophylactic anticonvulsants in moderate to severe head injury. Int J Emerg Med. 2010 Jul 22;3(3):187-91.
- ↑ Szaflarski JP et al. Prospective, randomized, single blinded comparative trial of intravenous levetiracetam versus phenytoin for seizure prophylaxis. Neurocrit Care 2010;12:165-172.
- ↑ Schulz-Stübner S: Sedation in traumatic brain injury: avoid etomidate. Crit Care Med. 2005, 33 (11): 2723.
- ↑ Marion DW, Penrod LE, Kelsey SF, et al: Treatment of traumatic brain injury with moderate hypothermia. New Engl J Med. 1997, 336: 540-546.
- ↑ Marion DW: Optimum serum glucose levels for patients with severe traumatic brain injury. F 1000 Med Rep. 2009, 1: 42.
- ↑ Roberts I, Yates D, Sandercock P, Farrell B, Wasserberg J, Lomas G, Cottingham R, Svoboda P, Brayley N, Mazairac G, Laloë V, Muñoz-Sánchez A, Arango M, Hartzenberg B, Khamis H, Yutthakasemsunt S, Komolafe E, Olldashi F, Yadav Y, Murillo-Cabezas F, Shakur H, Edwards P, CRASH trial collaborators: Effect of intravenous corticosteroids on death within 14 days in 10008 adults with clinically significant head injury (MRC CRASH trial): randomised placebo-controlled trial. Lancet. 2004, 364: 1321-1328.
- ↑ Haddad SH and Arabi YM. Critical care management of severe traumatic brain injury in adults. Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine 2012. 20:12.
- ↑ Kassell NF, Hitchon PW, Gerk MK, Sokoll MD, Hill TR: Alterations in cerebral blood flow, oxygen metabolism, and electrical activity produced by high dose sodium thiopental. Neurosurgery. 1980, 7: 598-603.