We need you! Join our contributor community and become a WikEM editor through our open and transparent promotion process.
Penetrating neck trauma
From WikEM
Contents
Background
- Defined by platysma violation
- Assume significant injury has occurred until proven otherwise
- Never probe neck wounds beneath the platysma (may disrupt hemostasis)
- Multiple structures are injured in 50%
- Stab wound can enter in one zone and damage another
- Missed esophageal injury is leading cause of delayed death
- GSW that crosses midline of 2x as likely to cause injuries to vital structures
- Blunt cervical vascular injury should be treated with systemic anticoagulation
- Penetrating injury rarely results in unstable fracture
Clinical Features
| Hard Signs | Soft Signs |
|---|---|
| Airway compromise | Subcutaneous emphysema |
| Air bubbling wound | Dysphagia, dyspnea |
| Expanding or pulsatile hematoma | Non-pulsatile, non-expanding hematoma |
| Active Bleeding | Venous oozing |
| Shock, compromised radial pulse | Chest tube air leak |
| Hematemesis | Minor hematemesis |
| Neuro Deficit/Paralysis/Cerebral ischemia | Paresthesias |
Differential Diagnosis
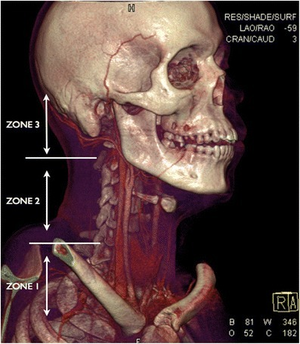
| Zone | Anatomic Landmarks | Potential Injuries |
|---|---|---|
| 1 | clavicle to cricoid |
|
| 2 | cricoid to angle of mandible |
|
| 3 | angle of mandible to base of skull |
|
Evaluation

Algorithm for CTA Neck after penetrating trauma][1]
Evaluation (WTA Algorithm)
- If hard signs or HD instability, attempt tamponade, secure airway, then OR.
- If no hard signs and yet suspect injury, CTA.
Imaging Options
- CXR
- Pneumo/hemothorax, pneumomediastinum
- CTA
- 1st line
- Angiography
- Gold-standard
- Useful if embolization or stent placement are anticipated or CT inconclusive
Management
General
- Airway
- If integrity of larynx is in question trach may be safer than intubation
- One attempt at intubation by most experienced provider with tube one size smaller[2]
- If failure, surgical airway should be performed
- Emergency tracheostomy preferred to cricothyrotomy
- Consider intubation if:
- Stridor
- Hemoptysis
- Subq emphysema
- Expanding hematoma
- Breathing
- Minimize BVM (positive pressure > air into soft tissue plains)
- Circulation
- Place IV on contralateral side of injury
- Disability
- Neuro deficits may be secondary to direct cord injury or cerebral ischemia secondary to carotid injury
- Place in C-collar if:
- ALOC, neuro deficits, or sig. blunt injury
By Zone
Zone I
- Portable CXR
- Evaluation is generally by selective, nonoperative management
- Vascular control can be difficult; requires thoracic surgical approach
Zone II
- Optimal management is controversial
- Platysma
- Not penetrated: obs and discharge
- Penetrated and vitals/airway stable: CT angio of neck
- Penetrated and unstable, expanding hematoma: OR
- Platysma
- All bleeding should be controlled with pressure, not with clamps
Zone III
- Treat as cranial injuries
- Evaluation is generally by selective, nonoperative management
- Routine exploration of zone III is not indicated
By Structure
Esophagus
- Injuries are often initially asymptomatic
- If missed can lead to neck space infection, mediastinitis
- Esophagoscopy or contrast esophagography indicated if:
- CT is equivocal or abnormal
- Missile trajectory places esophagus at risk for injury
- Persistent symptoms
Laryngotracheal
- Suspect if:
- Air bubbling through wound
- Dyspnea, stridor
- Hemoptysis
- Subcutaneous emphysema
- Laryngoscopy is indicated if:
- Suspect laryngotracheal injury even if CT is negative
Disposition
- If CT is negative, may observe patient
Disposition
See Also
References
- ↑ Sperry JL, Moore EE, Coimbra R, et al. Western Trauma Association critical decisions in trauma: penetrating neck trauma. J Trauma Acute Care Surg. 2013;75(6):936–940. [1]
- ↑ Newton K, Claudius I: Neck in Marx JA, Hockberger RS, Walls RM, et al (eds): Rosen’s Emergency Medicine: Concepts and Clinical Practice, ed 8. St. Louis, Mosby, Inc., 2013, (Ch) 44: pp 425-257.