We need you! Join our contributor community and become a WikEM editor through our open and transparent promotion process.
Pediatric fever of uncertain source
From WikEM
(Redirected from Pediatric fever)
Contents
Background
- Medicine is an art as well as science, practice clinical judgment when using guidelines
- Preemies: Count age by estimated postconception date (not by actual delivery date) for 1st-90d
| Age | 0-14 days | 14-28 days | 28-60 days (pre vaccine) | 28-60 days (post vaccine) | 60-90 days | > 90 days |
| Meningitis/SBI Prevalence | 1/10 | 1/20 | 1/100 | 1/1000 | 1/1000-10,000 | > 1/10,000 |
Facts and Figures
From ACEP's Clinical Policy on Pediatric Fevers[1]
- 7% of patients < 2 years old with fever have pneumonia, however the etiology (viral/bacterial) or even the presence of pneumonia has low inter-observer reliability even among pediatric radiologists
- 4% Prevalence of UTI with common other sources of fever (OM, viral URI, et cetera)
- 1.5-2% background prevalence of asymptomatic bacteruria in healthy afebrile controls
- 0.3% Rate of occult bactremia with healthy, well-appearing child who has a fever 2-24 months
- 0.3% of previously well children aged 3-36 months who have a fever without a source will develop significant sequelae, 0.03% will develop sepsis or meningitis
Concomitant RSV or Infulenza Infection
- In RSV+ (by PCR) neonates aged 0-28 days, 6.1% had UTIs and 3.7% were bactremic; there was no difference in rates of SBI between RSV+ and RSV- neonates in a large prospective multicenter study entailing 1,248 children[2]
- RSV+ infants aged 29-60 days, the SBI rate was 5.5%, all of which were UTIs
- Influenza+, low risk of bacterial illness
Differential Diagnosis
Pediatric fever
- Upper respiratory infection (URI)
- UTI
- Sepsis
- Meningitis
- Febrile seizure
- Pneumonia
- Acute otitis media
- Whooping cough
- Unclear source
- Kawasaki disease
- Neonatal HSV
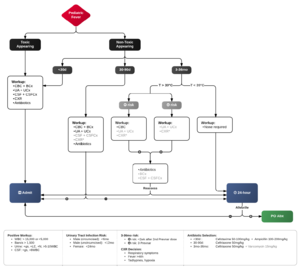
Evaluation & Management
0-28dy
| Child Appearance | Work Up | Treatment | Disposition & Follow-up | Comments |
| Temperature ≥38°
Toxic or Well |
|
|
Admit | SBI incidence
|
^Acyclovir if:
28dy-90dy[3]
| Appearance | Work Up | Treatment | Disposition & Follow-Up |
| Temp≥38° + Toxic |
|
|
Admit |
|
Temp≥°38 + Well |
|
|
Workup(+): Antibiotics and admit
Workup(-): ?antibiotics; home with 24 follow-up |
^^Can use ceftriaxone 50-100mg/kg, but concern for bilirubin displacement
- CXR for (use clinical judgment):
- Resp symptoms
- Fever >48 hrs
- Tachypnea
- Decreased SaO2
^Acyclovir if:
90dy-36mo[4]
| Appearance | Work Up | Treatment | Disposition & Follow-Up |
| T≥38° + Toxic |
|
|
Admit |
| T≥39°C + Well + Non-complete Prevnar |
|
If WBC(+):
|
Outpatient (24 hour follow-up) |
| T≥39°C + Well + Prevnar |
|
Treat cystitis or pneumonia if postitive | Outpatient (48hour follow up) |
| T≥38-38.9°C + Well | Consider UA, CXR based on symptoms, etc | Treat cystitis or pneumonia if positive | Outpatient (48-72 hour follow-up)[5] |
- CXR for (use clinical judgment):
- Resp symptoms
- Fever >48 hrs
- Tachypnea
- Decreased SaO2
Low Risk Lab Criteria
If low-risk criteria below not met, then perform the LP (if not done) and admit for inpatient antibiotics[6][7]
CBC
- WBC 5-15 /mm3
- Absolute Band count <1500 /mm3
Urinalysis
- Clear
- Neg Nitrate and Leukocyte esterase
- WBC <10/high powered field
CSF
0-28 days
- WBC: 0-22/mm3
- Protein: <100mg/dL
>29 days
- WBC 0-7/mm3
- Protein: 15-25mg/dL
Low Risk by Step-By-Step Approach[8]
Study validated against Rocheter criteria and Lab-score for identifying low risk for invasive bacterial infections (IBI), with NPV ~98%
- Well appearing
- Age > 21 days
- No leukocyturia
- Procalcitonin < 0.5 ng/mL
- ANC < 10,000/mm3
- CRP < 20 mg/L
Low Risk Management[9]
- Offer no LP, no antibiotics, 24 hrs observation
- Plan for prompt follow-up
Symptomatic Managment
Acetaminophen Pediatric Dosing Chart
| Weight (kg) | Weight (lbs) | Age | Dosage (mg) |
| 3-4 | 6-11 | 0-3 mo | 40 |
| 5-7 | 12-17 | 4-11 mo | 80 |
| 8-10 | 18-23 | 1-2 y | 120 |
| 11-15 | 24-35 | 2-3 y | 160 |
| 16-21 | 36-47 | 4-5 y | 240 |
| 22-26 | 48-59 | 6-8 y | 320 |
| 27-32 | 60-71 | 9-10 y | 400 |
| 33-43 | 72-95 | 11 y | 480 |
- Dosage can be given q6hours
See Also
- Acute fever
- Fever of unknown origin (peds)
- Urinary tract infection (peds)
- Sepsis (peds)
- Meningitis (peds)
- Febrile seizure
External Links
References
- ↑ Clinical Policy for Children Younger Than Three Years Presenting to the Emergency Department With Fever. Annuals of Emergency Medicine 2003 42. 530-545
- ↑ Greenes, D.S.M., & Harper, M. B.M. (1999). Low risk of bacteremia in febrile children with recognizable viral syndromes. Pediatric Infectious Disease Journal, 18(3), 258-261.
- ↑ Jaskiewicz, J.A., McCarthy, C.A., Richardson, A.C., White, K.C., Fisher, D.J., Powell, K. R., et al. (1994). Febrile infants at low risk for serious bacterial infection-an appraisal of the Rochester criteria and implications for management. Pediatrics 94(3), 390-396.
- ↑ Jaskiewicz, J.A., McCarthy, C.A., Richardson, A.C., White, K.C., Fisher, D.J., Powell, K. R., et al. (1994). Febrile infants at low risk for serious bacterial infection-an appraisal of the Rochester criteria and implications for management. Pediatrics 94(3), 390-396.
- ↑ Baker, M.D., Bello, L.M., & Avner, J.R. (1993). Outpatient management without antibiotics of fever in selected infants. New England Jouranl of Medicine, 329(20), 1437-1441.
- ↑ Smitherman, H.F. & Macias, C.G. (2014). Evaluation and management of fever in the neonate and young infant (less than three months of age) [Electronic Version]. UpToDate,Teach, S.J., Kaplan, SL, Wiley, JF.
- ↑ Dagan, R. Sofer, S., Phillip, M., & Shachak, E. (1988). Ambulatory care of febrile infants younger than 2 months of age classified as being at low risk for having serous bacterial infections. Journal of Pediatrics, 112(3), 355-360.
- ↑ Gomez B, Mintegi S, Bressan S, et al. Validation of the “Step-by-Step” Approach in the Management of Young Febrile Infants. Pediatrics. 2016;138(2):e20154381
- ↑ Mintegi S, Gomez B, Martinez-Virumbrales L, et al. Outpatient management of selected young febrile infants without antibiotics. Arch Dis Child. 2016 Jul 28. pii: archdischild-2016-310600. doi: 10.1136/archdischild-2016-310600.