We need you! Join our contributor community and become a WikEM editor through our open and transparent promotion process.
Missile embolus
From WikEM
Contents
Background
- Missle Embolization is an umbrella term encompassing the intravasculature and intracardiac embolization of bullet fragments, pellets, and shrapnel most commonly from war related penetrating traumas (mortars, grenades, mines, etc.)[1].
- A rare phenomenon with the majority of cases occurring in war/combat penetrating trauma, although civilian cases have been reported [2].
- Definitive recommendations regarding management and treatment are varied.
Clinical Features

Ct chest showing intracardiac missle emboli [1]

Intraoperative arteriogram identified a lumen occluding fragment in the axillary artery(arrow)[2]
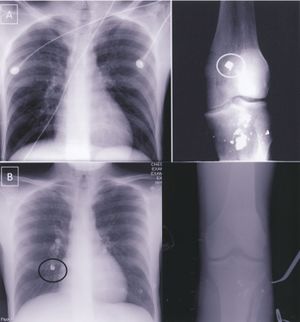
(B)Post operative CXR and plain films of the right knee demonstrate embolization of knee fragment to right lower lobe (black circle) when compared to preoperative films (A) [2]
- Commonly present with asymmetric peripheral pulses, evidence of metallic fragments remote from the site of penetrating injury (outside of the expected fragment trajectory), and lack of an exit wound [2].
- However, patient presentation can vary. Hemodynamically stable vital signs, lack of penetrating trauma on a pulseless extremity, and the presence of an exit wound should not be used to exclude the diagnosis.
- As delayed and occult arterial injury have been reported in the literature, serial imaging may be necessary if suspicion remains high in the absence of initial findings.
Arterial Missile Emboli Complications [3]
- Distal ischemia
- Thrombosis
- Further embolization
Venous Missile Emboli Complications
- Pulmonary artery embolism
- Cardiac valve dysfunction
- Endocarditis
- Abscess formation
- Sepsis
- Thrombosis
- Dysrhythmias
- Intraventricular communications
- Conduction defects
- Tissue erosion
- Hemorrhage
- Cardiac ischemia from erosion into coronary vessels
- Thrombophlebitis
Psychiatric Complications
- Anxiety
- Cardiac neurosis
- Fear of movement resulting in a dislodgment of the missile from its current location
Evaluation
Need high incidence of suspicion with penetrating trauma (up to 5% of arterial injuries may be missed on the initial CT angiogram in patients with fragmentation wounds) [1].
- CXR
- X-ray (location specific) and/or CT
- Look for evidence of metallic foreign bodies both near and far from the site of penetrating injury
- CT angiogram of the involved extremity, if evidence of extremity foreign body (e.g. diminished or absent pulses)
- If there is evidence of intracardiac or intrapulmonary foreign bodies, consider:[1]
- CT chest/abdomen/pelvis with IV contrast (to determin missile trajectory, size, and exact location).
- 2D transesophageal echocardiogram is also recommended for intrathoracic missiles.
Management
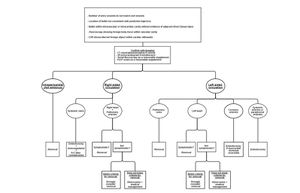
Algorithm for Management of Missile Emboli based on Anatomic Location[1]
- Remove symptomatic missile emboli
- Low threshold to remove asymptomatic missle emboli (since they can become dislodged and lead to other complications)
- Surgical management is case specific, but minimally invasive embolectomies are preferred if there is a high probability of missile retrieval [3].
- There is not strong evidence supporting prophylactic antibiotic use.
- However, patients with intracardiac emboli may benefit from 48 hours of a first generation cephalosporin to prevent endocarditis with the addition of an aminoglycoside for soft tissue cavitating injuries.
- Patients with retained missiles who are not surgical candidates maybe benefit from 12 months of anticoagulation [3].
Pitfalls in Management and Treatment[3].
- Delayed recognition
- Dislodgement of the missile during central venous catheter placements and/or inferior vena cava filters
- Repeated emobolization with patient reposition and surgical manipulation
Disposition
- Admission
See Also
References
- ↑ 1.0 1.1 1.2 1.3 1.4 Lu, K., Gandhi, S., Qureshi, M., Wright, A., Kantathut, N., & Noeller, T. (2015). Approach to Management of Intravascular Missile Emboli: Review of the Literature and Case Report. Western Journal of Emergency Medicine, 16(4), 489–496. http://doi.org/10.5811/westjem.2015.5.25553
- ↑ 2.0 2.1 2.2 2.3 Aidinian, G., Fox, C. J., Rasmussen, T. E., & Gillespie, D. L. (2010). Varied presentations of missile emboli in military combat. Journal of Vascular Surgery, 51(1), 214–217. http://doi.org/10.1016/j.jvs.2009.06.054
- ↑ 3.0 3.1 3.2 3.3 Singer, R. L., Dangleben, D. A., Salim, A., Kurek, S. J., Shah, K. T., Goodreau, J. J., … Szydlowski, G. W. (2003). Missile Embolism to the Pulmonary Artery: Case Report and Pitfalls of Management. Annals of Thoracic Surgery, 76(5), 1722–1725. http://doi.org/10.1016/S0003-4975(03)00692-1
