We need you! Join our contributor community and become a WikEM editor through our open and transparent promotion process.
Missile embolism
From WikEM
Contents
Background
- Also known as "bullet embolism"
- Occurs when a bullet or bullet fragment enters the bloodstream.
- Can be arterial (80%) or venous[1]
- Usually a small-caliber, low velocity projectile.[1]
- For this reason, incidence higher in non-military setting due to predominance of lower velocity projectiles
- Incidence = 1.1% in recent combat operations[2]
Clinical Features
- Number of entry wounds do not match exit wounds
- Location of bullet not consistent with predicted trajectory
- Bullet within intravascular or cavity without evidence of adjacent direct tissue injury
- Fluoroscopy showing foreign body move within vascular cavity
- CXR showing blurred foreign body within cardiac silhouette
Differential Diagnosis
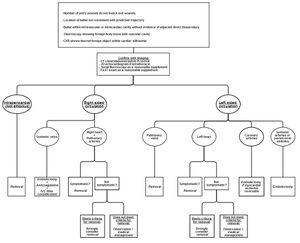
Missile embolism types
- Intrapericardial foreign body
- Systemic venous embolism
- Right heart and pulmonary artery embolism
- Pulmonary vein embolism
- Left heart embolism
- Coronary artery embolism
- Paradoxical embolus (due to patent foramen ovale)
Evaluation
- Need to maintain high index of suspicion, obtain full body radiography when indicated[1]
- TEE/TTE if intrathoracic
- Serial fluoroscopy, especially if intracardiac, but will not determine if buried in myocardium or free moving within cavity
- FAST exam as reasonable supplement
Management
- Controversial - not all need to be removed
- Refer to diagram / literature review references
Disposition
- Admit to trauma floor vs. ICU based on hemodynamic stability vs. risk of further embolism complication
See Also
References
- ↑ 1.0 1.1 1.2 Fernandez-Ranvier, Gustavo G. et al. Pulmonary artery bullet embolism—Case report and review. International Journal of Surgery Case Reports , Volume 4 , Issue 5 , 521 - 523
- ↑ Lu K et al. Approach to Management of Intravascular Missile Emboli: Review of the Literature and Case Report. West J Emerg Med. 2015 Jul; 16(4): 489–496.