We need you! Join our contributor community and become a WikEM editor through our open and transparent promotion process.
Insulin infusion device complication
From WikEM
Contents
Background
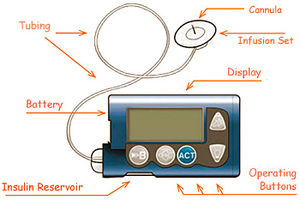
- Commonly used by patients with type 1 diabetes in the US
- External device connected by flexible tubing to a subcutaneous catheter
- Delivers continuous basal insulin and (by manually activating) bolus insulin (prandial or correction doses)
- Patient switches subcutaneous site every 3 days, refills insulin reservoir as needed every few days
Complications
- Hyperglycemia/DKA
- Due to failure to deliver insulin
- accidental (or iatrogenic) disconnection, kinked tubing, empty reservoir, uncharged batteries, poorly positioned needle, lipohypertrophy, patient not rotating sites
- DKA can occur very rapidly if pump fails, since pumps only use rapid-acting insulin
- Hypoglycemia
- Local complications
- Cellulitis[1], usually due to strep or staph
- Local reactions to adhesives or insulin preparation
- Lipohypertrophy
- Subcutaneous granulation tissue due to local insulin action
- May look/feel like an abscess
- Area has decreased sensation
- Infusing through such sites→ erratic insulin absorption→ labile blood glucose, hyperglycemia
Evaluation
- See Hyperglycemia and DKA
- See Hypoglycemia
- See Cellulitis
- Patients most often know how to operate and perform basic diagnostics on their pump
- Many devices have a log of bolus histories and changes to basal rates, alarms, etc.
- All major pump manufacturers have a 24/7 technical support hotline
Management
- Awake, alert patients without diabetes-related complaints should be allowed to operate their pump while in the ED
- If pump needs to be disconnected for >1hr, give a dose of subcutaneous insulin
- Hypoglycemia
- Do NOT disconnect pump
- Work up and treat as you would any other hypoglycemic patient
- Hyperglycemia
- Have patient administer an insulin bolus
- DKA
- Assume device failure
- Turn off and disconnect pump by pulling the catheter out from under the dressing removing it from the subcutaneous insertion site
- Continue usual DKA management
Disposition
See Also
External Links
References
- ↑ Richardson T, Kerr D. Skin-Related Complications of Insulin Therapy: Epidemiology and Emerging Management Strategies. Am J Clin Dermatol, 2003; 4 (10): 661-667
Authors
Claire, Ross Donaldson, Daniel Ostermayer, Neil Young, Michael Holtz