EBQ:ED Preoxygenation
PubMed PDF
Contents
Clinical Question
Reviews preoxygenation and peri-intubation oxygenation techniques to minimize the risk of critical hypoxia and introduces a risk-stratification approach to emergency tracheal intubation.
Major Points
- Prior to intubation, physicians should aim to achieve an 02 saturation of 100%
- Increasing oxygen storage requires denitrogenation of the residual capacity of the lungs
- Preoxygenation can extend the duration of time until a patient reaches O2 saturation of 88-90%. This is know as the “safe apnea” period.
- Desaturation after Paralysis with succinylcholine in adults (<90% O2 saturation)[1]
- 8.7 min in healthy patient (70kg)
- 5.5 minutes in moderately ill patient
- 3.7 minutes in healthy child (10kg)
- 3.1minutes in obese patient (127kg)
Design
This was a review of methods and approaches to preparing for intubation of patients with varying levels of risk of hypoxia from critical care, emergency medicine, and anesthesia literature.
Conclusion
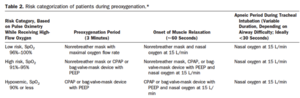
- Preoxygenation and apneic oxygenation are crucial in emergency airway management especially prior to rapid sequence intubation in order to prevent desaturation and prolong the time to desaturation, known as the safe apenic period.
- Since standard BVMs cannot deliver PEEP, in patients with shunt physiology (i.e. pneumonia, pulmonary edema, atelectasis) a PEEP valve attached to the BVM or non-invavisve positive pressure ventilation (i.e. CPAP,BIPAP) should be utilized
Preoxygenation Times:
- 3 minutes of tidal volume breathing with a high FiO2 source (15L nasal cannula + 100% non rebreather on patient at the same time)
- OR
- 8 vital capacity breaths (maximal inhalation and maximal exhalation) with a high FiO2 source
Oxygen Sources for Preoxygenation:
- Standard nonrebreather at 15L/minute will deliver 60 – 70% FiO2
- The FiO2 can be increased to ≥90% with flow rates > 30L/min
- OR
- Consider adding a nasal cannula increased >10L/min or as tolerated by patient along with nonrebreather mask
Positive pressure ventilation
- In patients unable to achieve oxygen saturations of >93 – 95% with 3 minutes of high FiO2
- In patients already apneic due to respiratory failure
- Should be used in patient's with shunt physiology to recruit alveoli
Patient Positioning
- Head elevation, chin lift, oropharyngeal airway and jaw thrust will ensure proper oxygenation during apnea
- Cricoid pressure should be avoided since it can cause tracheal compression hindering ventilation
- Patient should be positioned with ear to sternal notch
| 20° head-up | 386 vs 283 seconds to desaturate[2] |
| 20° head-up | 452 vs 364 seconds to desaturate[3] |
| 25° head-up for BMI > 40 | 214 vs 162 seconds to desaturate [4] |
Reverse Trendelenburg position (head of stretcher 30 degrees higher than the foot) in patients who cannot bend at the waist or shoulders or immobilized for possible spinal injury.
Paralytic Usage
The fasciculations induced by succinylcholine may cause increased oxygen use and favoring rocuronium may improve safe apenic period
Review Questions
Sources
- ↑ 1. Benumof JL, Dagg R, Benumof R. Critical Hemoglobin Desaturation Will Occur before Return to an Unparalyzed State following 1 mg/kg Intravenous Succinylcholine. Anesthesiology. 1997;87(4):979.
- ↑ Lane S, Saunders D, Schofield A, et al. A prospective, randomised controlled trial comparing the efficacy of pre- oxygenation in the 20 degrees head-up vs supine position. Anaesthesia. 2005;60:1064-1067
- ↑ Ramkumar V, Umesh G, Philip FA. Preoxygenation with 20° head- up tilt provides longer duration of non-hypoxic apnea than conventional preoxygenation in non-obese healthy adults. J Anesth. 2011;25:189-194
- ↑ Dixon BJ, Dixon JB, Carden JR, et al. Preoxygenation is more effective in the 25 degrees head-up position than in the supine position in severely obese patients: a randomized controlled study. Anesthesiology. 2005;102:1110-1115; discussion 1115A
Authors
Daniel Ostermayer, christina, Michael Lamberta, Ross Donaldson