We need you! Join our contributor community and become a WikEM editor through our open and transparent promotion process.
Difficult airway algorithm
From WikEM
(Redirected from Difficult Airway Algorithm)
Contents
LEMON Mnemonic
- An airway assessment score based on criteria of the LEMON method is able to successfully stratify the risk of intubation difficulty in the emergency department.[1]
LOOK
- Look at the patient externally for characteristics that are known to cause difficult laryngoscopy, intubation or ventilation[2]
- Trauma
- Short neck
- Micrognathia
- Prior surgery
- May also be difficult to bag
- Body mass index
- Advanced age
- Beard
- No teeth
- Snoring
- Dentures
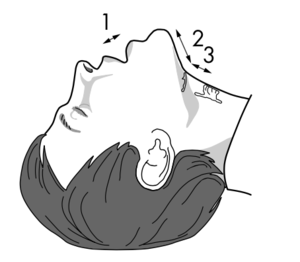
Evaluate 3-3-2-1
- 3 - Ideally the distance between the patient's incisor teeth should be at least 3 finger breadths
- 3 - Distance between the hyoid bone and the chin should be at least 3 finger breadths
- 2 - Distance between the thyroid notch and the floor of the mouth should be at least 2 finger breadths
- 1 - Lower jaw should not sublux more than 1cm
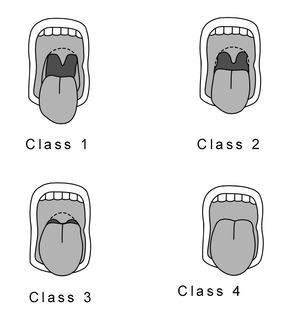
Mallampati
- The patient sits upright, opens mouth and protrudes tongue
- Grades are based on visibility of the uvula, posterior pharynx, hard, and soft palate
Obstruction
- Assess for conditions leading to airway obstruction such as Peritonsillar Abscess (PTA), trauma, or Epiglottitis.
Neck Mobility
- Patient places chin down onto their chest and extend their neck.
- Remove the hard collar and provide manual stabilization in trauma patients.
- Poor neck mobility impacts ability to have airway access alignment.
ASA Difficult Airway Algorithm
- Does not necessary apply to the ED since the patient can always be awakened and case cancelled
- Cricothyrotomy should always be the last step in patients with failure to oxygen and ventilate with BVM and inability to intubate
- Straight blade- Miller- may offer better manipulation of a large epiglottis in children or for micrognathia or "buck teeth"
Airway Adjuncts
Gum Bougie
- Blind orotracheal intubation
Blind Naso Trach Intubation
- Not as successful but still an option
- Higher complication rate - bleeding, emesis, and airway trauma
- Do not attempt in patients with posterior pharyngeal swelling such as in Angioedema (Upper Airway)
Lighted Optical Stylets
- High success rate - especially good for trauma, c-spine precautions
- Use for both reg and nasotrach
- Lower complication rate
- Limited by fogging, secretion, recognition of anatomy, cost, and rare provider experience
LMA
- Can use without muscle relaxants
- Better than face mask
- Can be used as bridge to fiberoptic intubation
- Limited by unreliable seal at peak insp pressure
- Aspiration risk
- Mucosal trauma
- LMA better than endotracheal for paramedics, especially in pediatric patients[3][4]
- Intubating LMA (LMA-Fastrach) provides the opportunity to convert to a definitive airway after rescue with the supraglottic device
Combitube- esoph obturator
- Good for nurses and paramedics with limited intubation skill
- Indicated if difficult airway predicted: cannot see glottis with laryngoscope
- Reduced risk for aspiration compared to face mask or LMA
- Can maintain spinal immobilization
- Large size predisposes to esophogeal dilatation and laceration as a complication
Percutaneous Transtracheal Ventilation
- PTV
- Prefered over crithyrotomy in children up to age 10-12
- Needle, 16-18ga through cricoid membrane, connected to 50 psi 02[5]
- Oxygenates well
- Ventilate through glottis and upper airway - can retain CO2
- Need adequate oxygen pressure
- 1 sec insp and 2- 3 sec exp to avoid breath stacking
- Can use for 30-45 min
- May cause pneumothorax or barotrauma
- Contraindications
- Distorted anatomy
- Bleeding diathesis
- Complete airway obstruction
Retrograde Intubation
- Percutaneous guide wire through cricoid and retrograde intubation over wire
- Use guide catheter over wire and then ett
- Need time to set up
- Risk hematoma, pneumothorax
- Contraindicated
- Bleeding
- Distorted anatomy
Fiberoptic Bronchoscopic Intubation
- Takes time to set up
- Good for c-spine injury or awake patient with diff airway
- Go through nose
- Use for all ages, can give 02 during procedure thru fiberscope, immediate confirmation of position
- Limited by secretions, bleeding, poor suction,
Rigid Fiberoptic Laryngoscopes
- Use for diff airway or spinal immobolization
- Not as good and longer time to intubate than flex scope
Improving Passive Oxygenation
- Use in overweight, poor O2 reserve, hypoxia at baseline, concerns for rapid progression to hypoxia once apnea
- Pre-oxygenate while sitting upright, only lay back once RSI drugs pushed.
- 30 degrees reverse trendelenburg position for intubation
- Nasal O2 while pre oxygenating and DURING intubation (after induction increase to 15L)
Surgical Airway
- Can get subglottic stenosis
- Rapid 4 step procedure faster but higher complication rate - cric cart fx
- Can also do wire guided
- Long term morbid, mortality similar to tracheostomy
See Also
- Intubation
- LMA
- ED Preoxygenation
- Cricothyrotomy
- Difficult airway algorithm
- Bag valve mask ventilation
Video
References
- ↑ Reed, M. et al. Can an airway assessment score predict difficulty at intubation in the emergency department? Emerg Med J. 2005 Feb; 22(2): 99–102. doi: 10.1136/emj.2003.008771
- ↑ Rennie LM, Dunn MJG, et al. Is the ‘LEMON’ method an easily applied emergency airway assessment tool? European Journal of Emergency Medicine 2004;11:154–7
- ↑ Zhu X-Y, Lin B-C, Zhang Q-S, Ye H-M, Yu R-J. A prospective evaluation of the efficacy of the laryngeal mask airway during neonatal resuscitation. Resuscitation. 2011;82(11):1405–1409. doi:10.1016/j.resuscitation.2011.06.010
- ↑ Calkins MD, Robinson TD. Combat trauma airway management: endotracheal intubation versus laryngeal mask airway versus combitube use by Navy SEAL and Reconnaissance combat corpsmen. J Trauma. 1999;46(5):927–932
- ↑ Beck, E., Kharasch, M., Casey, J., Ochoa, P., Menon, S., Calabrese, N. and Wang, E. (2011) ‘Percutaneous Transtracheal jet ventilation’, Academic Emergency Medicine, 18(5), pp. e38–e38.