Making Health Care Safer
Think sepsis. Time matters.
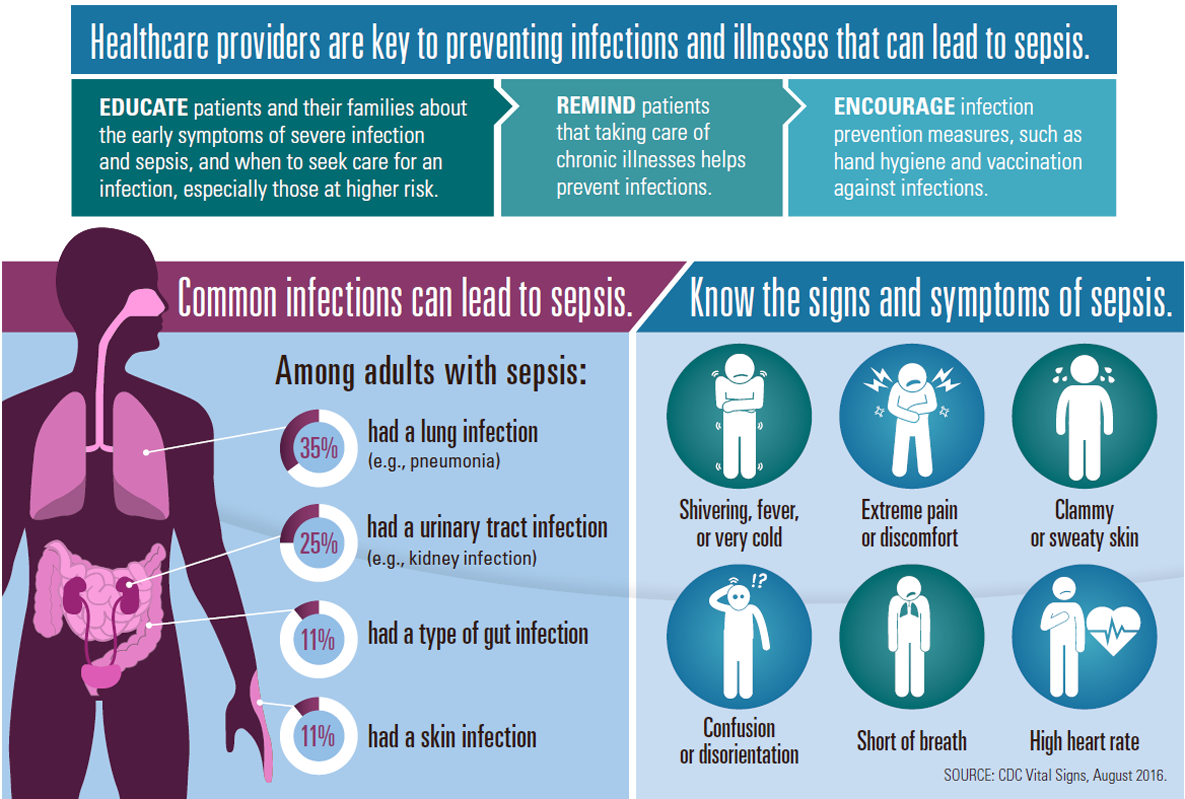
Healthcare providers are key to preventing infections and illnesses that can lead to sepsis.
- Educate patients and their families about the early symptoms of severe infection and sepsis, and when to seek care for an infection, especially those at higher risk.
- Remind patients that taking care of chronic illnesses helps prevent infections.
- Encourage infection prevention measures, such as hand hygiene and vaccination against infections.
Common infections can lead to sepsis.
Among adults with sepsis:
- 35% had a lung infection (e.g., pneumonia)
- 25% had a urinary tract infection (e.g., kidney infection)
- 11% had a type of gut infection
- 11% had a skin infection
Know the signs and symptoms of sepsis.
- Shivering, fever, or very cold
- Extreme pain or discomfort
- Clammy or sweaty skin
- Confusion or disorientation
- Short of breath
- High heart rate
SOURCE: CDC Vital Signs, August 2016.
Prevent sepsis and improve early recognition.
Improve health conditions.
George is a 72-year-old man with diabetes. During his check-up, George’s healthcare provider takes the opportunity to strengthen his chronic disease care (glucose control and skin care), provide recommended vaccines, and share information about symptoms that indicate an infection is worsening or sepsis is developing.
Educate patients and their families.
One month later, George has a cut on his foot that might be infected. He calls his healthcare provider, who tells him how to take care of the cut and signs of infection. Two days later, his foot is worse and he becomes short of breath, has clammy skin, and is more tired than usual. He recognizes symptoms are worsening and it could be sepsis. He seeks medical attention immediately.
Think sepsis. Act fast.
At the hospital, a healthcare provider recognizes the signs and symptoms of sepsis. She immediately orders tests to determine the source of infection and starts appropriate treatment, including antibiotics. She documents the dose, duration, and purpose of antibiotics.
Reassess patient management.
Healthcare providers closely monitor George’s progress and adjust therapy as needed. When George improves, his providers transfer him to a rehabilitation facility to continue his recovery. The hospital care team discusses his treatment plan with the team at the new facility.
SOURCE: CDC Vital Signs, August 2016.
- Page last reviewed: July 28, 2017
- Page last updated: July 28, 2017
- Content source:
- National Center for Emerging and Zoonotic Infectious Diseases
- Page maintained by: Office of the Associate Director for Communications (OADC)


 ShareCompartir
ShareCompartir