Preventing Teen Pregnancy
A Key Role for Health Care Providers
April 2015


 43%
43%
About 43% of teens ages 15 to 19 have ever had sex.
 4 in 5
4 in 5
More than 4 in 5 (86%) used birth control the last time they had sex.
 5%
5%
Less than 5% of teens on birth control used the most effective types.
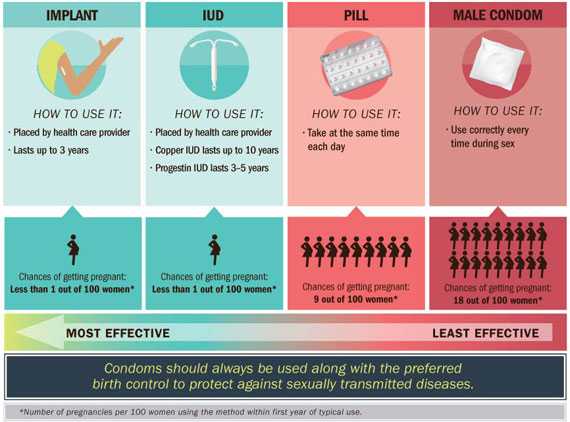
Teen childbearing can carry health, economic, and social costs for mothers and their children. Teen births in the US have declined, but still more than 273,000 infants were born to teens ages 15 to 19 in 2013. The good news is that more teens are waiting to have sex, and for sexually active teens, nearly 90% used birth control the last time they had sex. However, teens most often use condoms and birth control pills, which are less effective at preventing pregnancy when not used consistently and correctly. Intrauterine devices (IUDs) and implants, known as Long-Acting Reversible Contraception (LARC), are the most effective types of birth control for teens. LARC is safe to use, does not require taking a pill each day or doing something each time before having sex, and can prevent pregnancy for 3 to 10 years, depending on the method. Less than 1% of LARC users would become pregnant during the first year of use.
Doctors, nurses, and other health care providers can:
- Encourage teens not to have sex.
- Recognize LARC as a safe and effective choice of birth control for teens.
- Offer a broad range of birth control options to teens, including LARC, and discuss the pros and cons of each.
- Seek training in LARC insertion and removal, have supplies of LARC available, and explore funding options to cover costs.
- Remind teens that LARC by itself does not protect against sexually transmitted diseases and that condoms should also be used every time they have sex.
Problem
Few teens (ages 15 to 19) on birth control use the most effective types.
Use of Long-Acting Reversible Contraception (LARC) is low.
- Less than 5% of teens on birth control use LARC.
- Most teens use birth control pills and condoms, methods which are less effective at preventing pregnancy when not used properly.
- There are several barriers for teens who might consider LARC:
- Many teens know very little about LARC.
- Some teens mistakenly think they cannot use LARC because of their age.
- Clinics also report barriers:
- High upfront costs for supplies.
- Providers may lack awareness about the safety and effectiveness of LARC for teens.
- Providers may lack training on insertion and removal.
Providers can take steps to increase awareness and availability of LARC.
- Title X is a federal grant program supporting confidential family planning and related preventive services with priority for low-income clients and teens.*
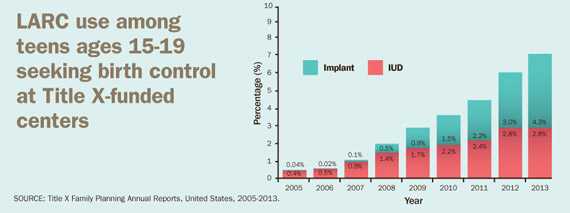
- Title X-funded centers have used the latest clinical guidelines on LARC, trained providers on LARC insertion and removal, and secured low- or no-cost options for birth control.
- Teen use of LARC has increased from less than 1% in 2005 to 7% in 2013.
- Other state and local programs have made similar efforts.
- More teens and young women chose LARC, resulting in fewer unplanned pregnancies.
LARC use among teens ages 15-19 seeking birth control at Title X-funded centers
SOURCE: Title X Family Planning Annual Reports, United States, 2005-2013.
Infographics
How does use of LARC vary by state among teens ages 15-19 seeking birth control at Title X-funded centers?
SOURCE: Title X Family Planning Annual Report, United States, 2013
View larger image and text description
How effective is LARC at preventing pregnancy compared with other birth control commonly used by teens?
SOURCE: Trussell J., Contraception, May 2011
What Can Be Done
The Federal government is
- Supporting efforts to prevent teen pregnancy by providing affordable family planning services.
- Developing clinical guidance for safe and effective use of birth control.
- Developing and evaluating programs in communities where teen births are highest.
Doctors, nurses, and other health care providers can
- Encourage teens not to have sex.
- Recognize LARC as a safe and effective first-line choice of birth control for teens, according to clinical guidelines for adolescents from the American College of Obstetricians and Gynecologists and the American Academy of Pediatrics.
- Offer a broad range of birth control options to teens, including LARC, and discuss the pros and cons of each.
- Seek training in LARC insertion and removal, have supplies of LARC available, and explore funding options to cover costs.
- Remind teens that LARC by itself does not protect against sexually transmitted disease sand that condoms should also be used every time they have sex.
Parents, guardians, and caregivers can
- Talk with their teens about sex, including:
- encouraging them not to have sex.
- encouraging them to use effective birth control to prevent pregnancy, along with condoms to protect against sexually transmitted diseases.
- Visit a health care provider with the teen to learn about various types of birth control, including LARC.
- Check with their health plan(s) about coverage of preventive services. Birth control and counseling may be available for teens at no out-of-pocket cost.
Teens can
- Choose not to have sex.
- Talk openly to parents or other trusted adults and ask how they can get birth control if they choose to be sexually active.
- Talk with a health care provider to learn about the best types of birth control for them, and use it and condoms correctly every time.
- Find a nearby clinic that provides birth control.
Science Behind the Issue
Related Pages
- Vital Signs Issue details: Trends in Use of Long-Acting Reversible Contraception Among Teens Aged 15–19 Years Seeking Contraceptive Services — United States, 2005–2013, Morbidity and Mortality Weekly Report (MMWR)
- Health Care Providers and Teen Pregnancy Prevention
- CDC Contraceptive Guidance for Health Care Providers
- Winnable Battles: Teen Pregnancy
- Prevention Status Reports (PSRs): Teen Pregnancy
- FastStats: Teen Births
- Vital Signs – Preventing Teen Pregnancy [PODCAST – 1:15 minutes]
- Vital Signs – Preventing Teen Pregnancy [PSA – 0:60 seconds]
On Other Web Sites
- Page last reviewed: April 7, 2015
- Page last updated: April 7, 2015
- Content source:
- National Center for Chronic Disease Prevention and Health Promotion, Division of Reproductive Health
- Page maintained by: Office of the Associate Director for Communications (OADC)


 ShareCompartir
ShareCompartir