Making Health Care Safer
Antibiotic Rx in Hospitals: Proceed with Caution
 1 in 2
1 in 2
More than half of all hospital patients receive an antibiotic.
 3x
3x
Doctors in some hospitals prescribed 3 times as many antibiotics as doctors in other hospitals.
 30%
30%
Reducing the use of high-risk antibiotics by 30% can lower deadly diarrhea infections by 26%.
Antibiotics save lives, but poor prescribing practices are putting patients at unnecessary risk for preventable allergic reactions, super-resistant infections, and deadly diarrhea. Errors in prescribing decisions also contribute to antibiotic resistance, making these drugs less likely to work in the future.
To protect patients and preserve the power of antibiotics, hospital CEOs/medical officers can:
- Adopt an antibiotic stewardship program that includes, at a minimum, this checklist:
- Leadership commitment: Dedicate necessary human, financial, and IT resources.
- Accountability: Appoint a single leader responsible for program outcomes. Physicians have proven successful in this role.
- Drug expertise: Appoint a single pharmacist leader to support improved prescribing.
- Act: Take at least one prescribing improvement action, such as requiring reassessment within 48 hours to check drug choice, dose, and duration.
- Track: Monitor prescribing and antibiotic resistance patterns.
- Report: Regularly report to staff prescribing and resistance patterns, and steps to improve.
- Educate: Offer education about antibiotic resistance and improving prescribing practices.
- Work with other health care facilities to prevent infections, transmission, and resistance.
Problem
Poor antibiotic prescribing harms patients
Antibiotic prescribing practices vary widely and errors are common.
- About half of patients receive an antibiotic for at least one day during the course of an average hospital stay.
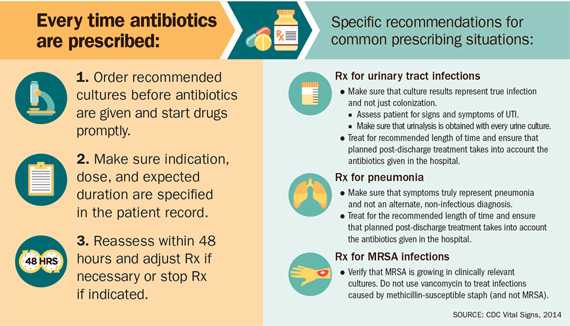
- The most common types of infections for which hospital clinicians wrote antibiotic prescriptions were lung infections (22%), urinary tract infections (14%), and suspected infections caused by drug-resistant Staphylococcus bacteria, such as MRSA (17%).
- About 1 out of 3 times, prescribing practices to treat urinary tract infections and prescriptions for the critical and common drug vancomycin included a potential error – given without proper testing or evaluation, or given for too long.
- Doctors in some hospitals prescribed up to 3 times as many antibiotics as doctors in similar areas of other hospitals. This difference suggests the need to improve prescribing practices.
Poor prescribing puts patients at risk.
- Although antibiotics save lives (for example, in the prompt treatment of sepsis, a life-threatening infection throughout the body), they can also put patients at risk for a Clostridium difficile infection, deadly diarrhea that causes at least 250,000 infections and 14,000 deaths each year in hospitalized patients.
- Decreasing the use of antibiotics that most often lead to C. difficile infection by 30% (this is 5% of overall antibiotic use) could lead to 26% fewer of these deadly diarrheal infections. These antibiotics include fluoroquinolones, β-lactams with β−lactamase inhibitors, and extended-spectrum cephalosporins.
- Patients getting powerful antibiotics that treat a broad range of infections are up to 3 times more likely to get another infection from an even more resistant germ.
SOURCE: CDC Vital Signs, 2014
SOURCE: CDC Vital Signs, 2014
What Can Be Done
Federal government is
- Expanding the National Healthcare Safety Network to help hospitals track antibiotic use and resistance.
- Sharing prescribing improvement recommendations and tools with clinicians and administrators. www.cdc.gov/getsmart/healthcare
- Supporting networks testing new prescribing improvement strategies.
- Helping hospitals and health departments create regional programs to improve antibiotic prescribing.
- Improving health care for veterans by launching antibiotic stewardship programs in Veteran’s Health Administration hospitals.
- Providing incentives for development of new antibiotics.
State and local health departments can
- Gain an understanding of antibiotic stewardship activities in the state or area.
- Facilitate efforts to improve antibiotic prescribing and prevent antibiotic resistance.
- Provide educational tools to facilities to help prescribers improve practices.
Hospital CEOs/medical officers can
- Adopt an antibiotic stewardship program that includes, at a minimum, this checklist [PDF – 425 KB]:
- Leadership commitment: Dedicate necessary human, financial, and IT resources.
- Accountability: Appoint a single leader responsible for program outcomes. Physicians have proven successful in this role.
- Drug expertise: Appoint a single pharmacist leader to support improved prescribing.
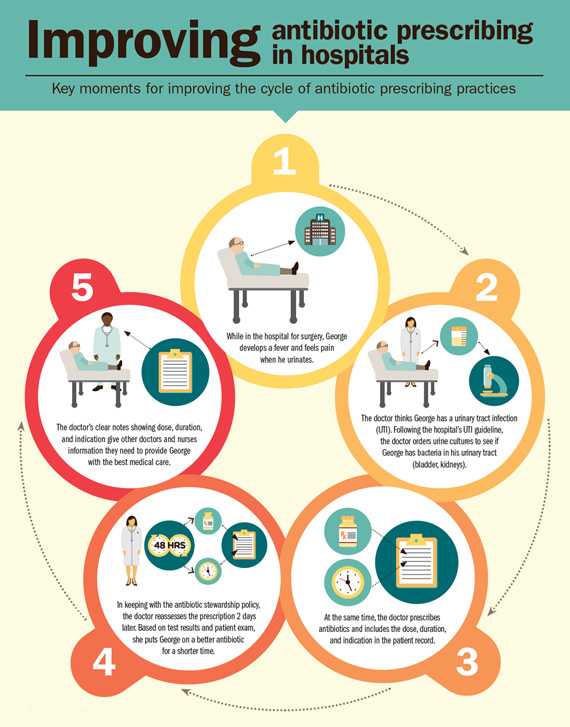
- Act: Take at least one prescribing improvement action, such as requiring reassessment within 48 hours, to check drug choice, dose, and duration.
- Track: Monitor prescribing and antibiotic resistance patterns.
- Report: Regularly report to staff prescribing and resistance patterns, and steps to improve.
- Educate: Offer education about antibiotic resistance and improving prescribing practices.
- Work with other health care facilities to prevent infections, transmission, and resistance.
Doctors and other hospital staff can
- Prescribe antibiotics correctly – get cultures, start the right drug promptly at the right dose for the right duration. Reassess the prescription within 48 hours based on tests and patient exam.
- Document the dose, duration and indication for every antibiotic prescription.
- Stay aware of antibiotic resistance patterns in your facility.
- Participate in and lead efforts within your hospital to improve prescribing practices.
- Follow hand hygiene and other infection control measures with every patient.
Hospital patients can
- Ask if tests will be done to make sure the right antibiotic is prescribed.
- Be sure everyone cleans their hands before touching you. If you have a catheter, ask each day if it is necessary.
Science Behind the Issue
Related Pages
- Vital Signs Issue details: Improving Antibiotic Use Among Hospitalized Patients, Morbidity and Mortality Weekly Report (MMWR)
- Vital Signs Press Release
- Vital Signs Digital Press Kit
- Checklist for Core Elements of Hospital Antibiotic Stewardship Programs
- Core Elements of Hospital Antibiotic Stewardship Programs
- Get Smart for Healthcare site
- HAI Prevention Stories from the States – South Dakota Improves Antibiotic Prescribing Practices [PDF – 377 KB]
- HAI Prevention Stories from the States – Improving Inpatient Antibiotic Prescribing Practices Across Georgia [PDF – 421 KB]
- Antibiotic RX in Hospitals: Proceed with Caution [PODCAST – 1:15 minutes]
- Antibiotic RX in Hospitals: Proceed with Caution [PSA – 0:60 seconds]
- CDC Healthcare-associated Infection Website
- Public Health Grand Rounds – Combating Resistance: Getting Smart About Antibiotics
On Other Web Sites
- Toolkit for Reduction of Clostridium difficile Infections Through Antimicrobial Stewardship
- CDC Foundation – Your Employees at Risk: Why Safe Healthcare is Everyone’s Business
- Dr. Frieden Medscape Commentary – Antibiotic Prescribing in Hospitals: Improvements Needed
- MedlinePlus – Antibiotics
- The Doctor’s Channel – Tom Frieden with Steps Doctors and
Hospitals Should Take - The Health Care Blog – Tom Frieden on Safer Patient Care
- MedPage Today – Tom Frieden Discusses Antibiotic Resistance in Hospitals
- Page last reviewed: March 4, 2014
- Page last updated: March 12, 2014
- Content source:
Error processing SSI file


 ShareCompartir
ShareCompartir