6|18 State Medicaid Agency Activities
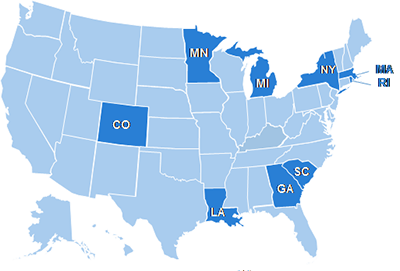 CDC is partnering with 9 State Medicaid Agencies to improve and accelerate implementation of the 6|18 interventions to achieve better care, better health outcomes, and lower costs.
CDC is partnering with 9 State Medicaid Agencies to improve and accelerate implementation of the 6|18 interventions to achieve better care, better health outcomes, and lower costs.
These 9 states have the potential to reach up to 17 million Medicaid enrollees with prevention interventions that work.
The initial focus for this collaboration is on 3 of the 6 health conditions -
asthma
,
tobacco use
, and
unintended pregnancy
- because these conditions are particularly prevalent among Medicaid beneficiaries. CDC’s goals in working with 9 State Medicaid Agency-Public Health Department teams are to understand best practices to implement 6|18 interventions in a State Medicaid Agency setting, and to help disseminate them to other states.
The 9 states had the following factors critical for success:
- They had active efforts in place to control one or more of the 3 priority health conditions.
- They were working to implement the specific interventions highlighted within the set of 18.
- The state supported the Medicaid Agency and the Department of Public Health working on this initiative in partnership.
Progress
State Medicaid Agency and Health Department teams in these 9 states are making tangible progress towards adoption of select interventions from among the 18. This includes participation in a Shared Learning Platform to facilitate peer-to-peer learning across states, where states have identified priorities such as the development of State Plan Amendments to broaden coverage of services, and the assessment of baseline coverage of interventions among managed care organizations as a first step towards contract negotiations.
Technical Assistance
CDC, the Centers for Medicare & Medicaid Services (CMS), and the Health and Human Services’ Office of the Assistant Secretary for Health (OASH) and Office of Population Affairs (OPA), along with the Health Resources and Services Administration (HRSA), the Association of State and Territorial Health Officials (ASTHO), and the National Association of Medicaid Directors (NAMD), are collaborating to support and provide technical assistance to state Medicaid programs. Best practices on how to most effectively use existing covered interventions will be shared with other state Medicaid Agencies. States use their own discretion to determine coverage for adult preventive services, since provision of preventive services for adults is optional under state Medicaid plans. State Medicaid programs receive targeted technical assistance and opportunities for peer learning to support implementation through CDC, in partnership with the Robert Wood Johnson Foundation and the Center for Health Care Strategies. Technical assistance includes:
- Individual monthly calls to discuss progress and identify challenges and technical assistance needs.
- Facilitated peer-to-peer learning calls focused on topics specific to each health condition held every other month.
- Webinars that address cross-cutting topics of interest to all states held on a quarterly basis.
Evaluation
CDC will work with health care purchasers, health plans, and providers who are implementing the specific interventions to monitor the quantitative, qualitative, and health and cost impact changes that occur as a result of this initiative.
Partner Support
CDC is leading the 6|18 Initiative with support from CMS, HRSA, and OASH/OPA. CMS has introduced 6|18 interventions as an option for integrating population health with delivery system transformation and payment reforms.
- Page last reviewed: September 28, 2016
- Page last updated: September 28, 2016
- Content source:


 ShareCompartir
ShareCompartir