
About Rural Health
Children in rural areas also face challenges. A recent CDC study finds that children in rural areas with mental, behavioral, and developmental disorders face more community and family challenges than children in urban areas with the same disorders.
These challenges highlight the need for additional attention and resources aimed at improving health in rural America. Rural areas could benefit from improved public health programs that support healthier behaviors and neighborhoods, and better access to healthcare services.
Why are rural Americans at greater risk for poor health outcomes?
Some rural areas have characteristics that put residents at higher risk of death, such as long travel distances to specialty and emergency care or exposures to specific environmental hazards.
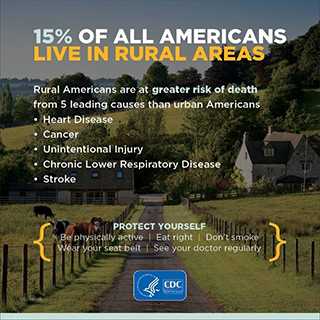
Rural Americans tend to have higher rates of cigarette smoking, high blood pressure, and obesity. Rural residents report less leisure-time physical activity and lower seatbelt use than their urban counterparts. They also have higher rates of poverty, less access to healthcare, and are less likely to have health insurance. All of these factors can lead to poor health outcomes.
What can be done to improve the health of rural Americans?
The gaps in health in rural areas can be addressed. For example, healthcare providers in rural areas can:
- Screen patients for high blood pressure and make blood pressure control a quality improvement goal. High blood pressure is a leading risk factor for heart disease and stroke.
- Increase cancer prevention and early detection. Rural healthcare providers should participate in the state-level comprehensive control coalitions. Comprehensive cancer control programs focus on cancer prevention, education, screening, access to care, support for cancer survivors, and overall good health.
- Encourage physical activity and healthy eating to reduce obesity. Obesity has been linked to a variety of serious chronic illnesses, including diabetes, heart disease, cancer, and arthritis.
- Promote smoking cessation. Cigarette smoking is the leading cause of preventable disease and death in the United States and is the most significant risk factor for chronic lower respiratory disease.
- Identify additional support for families who have children with mental, behavioral, or developmental disorders. Children with these issues would benefit from increased access to mental and behavioral healthcare; programs that support parents and caregivers; and increased opportunities to learn, play, and socialize. Because children in rural areas with these disorders more often experience financial difficulties, poor parental mental health, and a lack of neighborhood resources, these children may need additional support.
- Promote motor vehicle safety. Rural healthcare providers should encourage patients to always wear a seat belt and counsel parents and child care providers to use age- and size-appropriate car seats, booster seats, and seat belts on every trip.
- Engage in safer prescribing of opioids for pain. Healthcare providers should follow the CDC guideline when prescribing opioids for chronic pain and educate patients on the risks and benefits of opioids and using nonpharmacologic therapies to provide greater benefit.
- Page last reviewed: August 2, 2017
- Page last updated: August 2, 2017
- Content source:


 ShareCompartir
ShareCompartir