MRSA and the Workplace
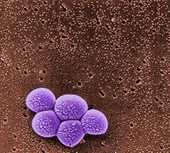
Source: CDC MRSA photos
Overview
Staphylococcus aureus, often referred to simply as “staph,” is a type of bacteria commonly carried on the skin or in the nose of healthy people. Sometimes, staph can cause an infection. Staph bacteria are one of the most common causes of skin infections in the United States. Most of these skin infections are minor (such as pustules and boils) and can be treated without antibiotics. However, staph bacteria also can cause serious infections (such as skin and soft tissue wound infections, bloodstream infections, and pneumonia).
Methicillin-resistantStaphylococcus aureus (MRSA) refers to types of staph that are resistant to a type of antibiotic methicillin. MRSA is often resistant to other antibiotics, as well. While 33% of the population is colonized with staph (meaning that bacteria are present, but not causing an infection with staph), approximately 1% is colonized with MRSA.
Workers who are in frequent contact with MRSA and staph-infected people and animals are at risk of infection. These included those in hospitals and healthcare facilities, correctional facilities, daycare facilities, livestock settings, and veterinary clinics.



FAQs for the Workplace
NOTE: This information is provided for general workplaces, not healthcare facilities. Healthcare workers should refer to information found at the following links: /mrsa/index.html and /mrsa/healthcare/index.html .
Can I get MRSA from my work?
MRSA is transmitted most frequently by direct skin-to-skin contact or contact with shared items or surfaces (e.g., towels, used bandages) that have come into contact with someone else's infected site. Animals with MRSA can also transfer the infection to people who frequently handle them. However, people are usually the originating source of the infection in animals.
MRSA skin infections can occur in any type of workplace. However, some workplace settings have factors that make it easier for MRSA to be transmitted. These factors, referred to as the 5 C's, are as follows: Crowding, frequent skin-to-skin Contact, Compromised skin (i.e., cuts or abrasions), Contaminated items and surfaces, and lack of Cleanliness. Locations where the 5 C's are common include schools, dormitories, military barracks, athletic gyms, households, correctional facilities, daycare centers, and areas where animal handling is common, such as veterinary clinics and livestock settings.
If I have MRSA, can I go to work?
Unless directed by a healthcare provider, workers with MRSA infections should not be routinely excluded from going to work.
Exclusion from work should be reserved for those with wound drainage (“pus”) that cannot be properly covered and contained with a clean, dry bandage and for those who cannot maintain good hygiene practices.
Workers with active infections should be excluded from activities where skin-to-skin contact with the affected skin area is likely to occur until their infections are healed.
What should I do if I think I have a staph or MRSA infection?
See your healthcare provider and follow your healthcare provider's advice about returning to work.
If I have staph, or a MRSA skin infection, what can I do to prevent the spread of MRSA at work and at home?
You can prevent spreading staph or MRSA skin infections to others by following these steps:
- Cover your wound.Keep areas of the skin affected by MRSA covered. Keep wounds that are draining or have pus covered with clean, dry bandages. Follow your healthcare provider's instructions on proper care of the wound. Pus from infected wounds can contain staph and MRSA, so keeping the infection covered will help prevent the spread to others. Bandages or tape can be discarded with the regular trash.
- Clean your hands.You, your family, and others in close contact should wash their hands frequently with soap and warm water or use an alcohol-based hand sanitizer, especially after changing the bandage or touching the infected wound.
- Do not share personal items.Avoid sharing personal items such as uniforms, personal protective equipment, clothing, towels, washcloths or razors that may have had contact with the infected wound or bandage.
- Talk to your doctor.Tell any healthcare providers who treat you that you have or had a staph or MRSA skin infection.
What should I do if I suspect that my uniform, clothing, personal protective equipment or workstation has become contaminated with MRSA?
Wash uniforms, clothing, sheets and towels that become soiled with water and laundry detergent. Drying clothes in a hot dryer, rather than air-drying, also helps kill bacteria in clothes. Use a dryer to dry clothes completely. Wash clothing according to manufacturer's instructions on the label.
Cleaning contaminated equipment and surfaces with detergent-based cleaners or Environmental Protection Agency (EPA)-registered disinfectants is effective at removing MRSA from the environment. Check the disinfectant product’s label on the back of the container. Most, if not all, disinfectant manufacturers will provide a list of microorganisms on their label that their product can destroy. Because cleaners and disinfectants can be irritating and exposure has been associated with health problems such as asthma, it is important to read the instruction labels on all cleaners to make sure they are used safely and appropriately. Where disinfection is concerned, more is not necessarily better. EPA has guidance for employers for less hazardous antimicrobial products
Additional information is available on effective infection-control practices while minimizing the use of, and exposure to, toxic products in schools written by the National Cleaning for Healthier Schools and Infection Control Workgroup.
Environmental cleaners and disinfectants should not be used to treat infections. The EPA provides a list of EPA-registered products effective against MRSA: http://epa.gov/oppad001/list_h_mrsa_vre.pdf.
What can my boss (employers) do to prevent the spread of staph or MRSA at the workplace?
- Place importance on worker safety and health protection in the workplace
- Ensure the availability of adequate facilities and supplies that encourage workers to practice good hygiene
- Ensure that routine housekeeping in the workplace is followed
- Ensure that contaminated equipment and surfaces are cleaned with detergent-based cleaners or Environmental Protection Agency (EPA)-registered disinfectants
- Encourage workers to seek early treatment of possible infections from their healthcare provider
Other FAQs About MRSA
Signs and Symptoms
What does a staph or MRSA infection look like?
Staph bacteria, including MRSA, can cause skin infections that may look like a pimple or boil and can be red, swollen, painful, or have pus or other drainage. More serious infections may cause pneumonia, bloodstream infections, or skin and soft tissue wound infections.


Source: CDC MRSA photos
Prevention
How can I prevent staph or MRSA skin infections?
Practice good hygiene:
- Keep your hands clean by washing thoroughly with soap and water or using an alcohol-based hand sanitizer.
- Keep cuts and scrapes clean and covered with a bandage until healed.
- Avoid contact with other people's wounds or bandages.
- Avoid sharing personal items such as uniforms and personal protective equipment.
- Avoid use of whirlpools and swimming pools if you have MRSA
Treatment
Are staph and MRSA infections treatable?
Yes. Many staph skin infections may be treated by draining the abscess or boil and may not require antibiotics. Drainage of skin boils or abscesses should only be done by a healthcare provider. Do not try to drain the infection yourself.
However, some staph and MRSA infections are treated with antibiotics. If you are given an antibiotic, take all of the doses, even if the infection is getting better, unless your doctor tells you to stop taking it. Do not share antibiotics with other people or save unfinished antibiotics to use at another time.
If after visiting your healthcare provider the infection is not getting better after 48 hours, contact them again. If other people you know or live with get the same infection tell them to go to their healthcare provider. MRSA skin infections can develop into more serious infections.
Preventing the Spread of MRSA in Correctional Facilities
NIOSH has created 14 easy-to-read publications on how to stop the spread of MRSA in correctional facilities. The title of each publication indicates the target audience. Conditions at correctional facilities can be conducive to the spread of MRSA, and several outbreaks have been reported. The materials cover a number of topics, including basic facts about MRSA, what to do if you have a skin infection, hand hygiene, personal protective equipment, environmental sanitation, laundry, and not sharing personal items.
Washing Your Hands Stops MRSA (Inmates)
DHHS (NIOSH) Publication No. 2013-113 (January 2013)
En Español
/spanish/niosh/docs/2013-113_sp/
Washing Your Hands Stops MRSA (Correctional Staff)
DHHS (NIOSH) Publication No. 2013-114 (January 2013)
Use Hand Sanitizer, Bottle (Correctional Staff)
DHHS (NIOSH) Publication No. 2013-115 (January 2013
Use Hand Sanitizer, Wall-Mounted Dispenser (Correctional Staff)
DHHS (NIOSH) Publication No. 2013-116 (January 2013)
What is MRSA? (Correctional Officers)
DHHS (NIOSH) Publication No. 2013-117 (January 2013)
What is MRSA? (Inmates)
DHHS (NIOSH) Publication No. 2013-118 (January 2013)
En Español
/spanish/niosh/docs/2013-118_sp/
What is MRSA? (Correctional Staff)
DHHS (NIOSH) Publication No. 2013-119 (January 2013)
Managers: Protect Correctional Staff from MRSA
DHHS (NIOSH) Publication No. 2013-120 (January 2013)
Managers' Checklist for Protecting Correctional Staff from MRSA
DHHS (NIOSH) Publication No. 2013-121 (January 2013)
Handle Laundry Safely (Correctional Facilities)
DHHS (NIOSH) Publication No. 2013-122 (January 2013)
En Español
/spanish/niosh/docs/2013-122_sp/
Use Personal Protective Equipment (Correctional Staff)
DHHS (NIOSH) Publication No. 2013-123 (January 2013)
MRSA Can Live on High-Touch Surfaces (Correctional Facilities)
DHHS (NIOSH) Publication No. 2013-124 (January 2013)
Sharing Personal Items Can Spread MRSA (Correctional Staff)
DHHS (NIOSH) Publication No. 2013-125 (January 2013)
If You Have a MRSA Infection (Correctional Staff)
DHHS (NIOSH) Publication No. 2013-126 (January 2013)
Additional Resources
MRSA and the Workplace
DHHS (NIOSH) Publication No. 2013-112 (January 2013)
This two-page factsheet summarizes information about MRSA and the workplace.
Environmental Cleaning and Disinfecting for MRSA
Veterinary Health Care and the Workplace
- Page last reviewed: August 17, 2015
- Page last updated: July 14, 2016
- Content source:
- National Institute for Occupational Safety and Health Education and Information Division


 ShareCompartir
ShareCompartir