Healthcare Response Activities
Read the full treatment recommendations for melioidosis in Emerging Infectious Diseases
If there is ever an emergency caused by the release of B. pseudomallei, hospitals and other healthcare facilities will be called upon to diagnose, treat, and care for patients with melioidosis.
Treat and Care for Patients
All patients with melioidosis will need to be treated with the appropriate antibiotic treatment regimen. Treatment consists of two rounds: an intravenous round and an oral eradication round. The first round of treatment usually lasts a minimum of 10 to 14 days, but may last up to 4 to 6 weeks for patients with more severe disease. The follow-on oral eradication round lasts 3 to 6 months.
Some patients may require intensive care, including ventilator support. Depending upon the scale of the emergency event, your healthcare facility may have many patients requiring intensive care for several days or weeks.
In an emergency, communicate with your state public health department’s Medical Countermeasures Coordinator to request additional supplies, such as ventilators, from the Strategic National Stockpile.
Identify Patients for Diagnostic Testing
Depending upon the circumstances of the emergency, some individuals who developed symptoms soon after coming into contact with B. pseudomallei, but before the emergency was identified, may have been diagnosed as having illnesses other than melioidosis. Healthcare facilities may need to work with public health authorities to perform tasks such as chart reviews to identify and contact individuals who require further testing and treatment.
Infection Control
Healthcare workers should follow standard precautions when caring for patients with melioidosis. Melioidosis is not considered to be transmitted person-to-person via air or respiratory droplets in non-laboratory settings. There have only been a few documented cases of person-to-person transmission; percutaneous inoculation is probably the most frequent route for natural infection.
Environmental Control
Current practices to disinfect and sterilize patient-care equipment and environmental surfaces are sufficient for managing areas where melioidosis patients are evaluated, admitted, and treated.
Protect Laboratory Staff
Laboratory personnel who handle specimens from patients suspected of having melioidosis or cultures of B. pseudomallei are at risk of laboratory-acquired melioidosis. In contrast to other healthcare personnel, laboratory personnel are at risk because some procedures required to prepare specimens for culture may aerosolize particles and release B. pseudomallei into the air. Laboratory personnel who have been exposed to B. pseudomallei should begin post-exposure prophylaxis immediately.
Laboratory personnel can reduce their risk of exposure by following good laboratory practices. Some precautions laboratory personnel should take:
- Perform work with clinical specimens using Biosafety Level 2 (BSL-2) practices*
- Always use appropriate personal protective equipment when working with the specimens or cultures
- Perform work with cultures or any tasks that generate aerosols or droplets in BSL-3 facilities
- Respiratory protection is essential when centrifuging or performing any other tasks outside of a biological safety cabinet (BSC)
*Clinical diagnostic laboratories functioning at BSL-2 may isolate B. pseudomallei from patient specimens. Once B. pseudomallei is suspected, transfer work to BSL-3 facilities.
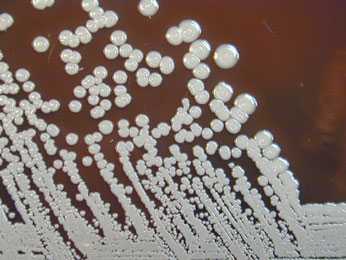
Photo source: CDC, Courtesy of Larry Stauffer, Oregon State Public Health Laboratory
Laboratory-related exposure
If a laboratory worker is exposed to B. pseudomallei, immediately wash and decontaminate the inoculation site (if there is one). Report the incident to the laboratory safety manager, and perform a risk assessment to determine whether the incident poses a low-risk or a high-risk.
Learn how to manage an accidental laboratory exposure to B. pseudomallei
The type of exposure determines the course of post-exposure management, summarized here:
| Type of exposure | Post-exposure Management |
|---|---|
| High-risk incident | Begin post-exposure prophylaxis immediately
Fever monitoring |
| Low-risk incident, with known risk factors for natural melioidosis | Begin post-exposure prophylaxis immediately
Fever monitoring |
| Low-risk incident, without known risk factors for natural melioidosis | Fever monitoring only |
Laboratory workers who have been exposed to B. pseudomallei should record their temperatures twice a day for 21 days (fever monitoring). Workers who were exposed and develop any of the following symptoms should seek medical care immediately and inform their clinician about their exposure to B. pseudomallei:
- Fever greater than 100.4°F (38°C)
- Cough
- Progressive inflammation at the site of known inoculation
- Page last reviewed: August 8, 2017
- Page last updated: August 8, 2017
- Content source:


 ShareCompartir
ShareCompartir