Clinical Case Study 2: 6-Week-Old Infant With Fever
(contributed by Prof. Jacques Le Bras, Hôpital Bichat - Claude Bernard, Paris, France)
A 30 year-old woman, HIV-positive, delivers by planned cesarean section an apparently normal female baby, weight 3.2 kg (7 lbs). At delivery AZT is administered IV for 7 hours. The mother is a native of the Democratic Republic of Congo who came to France 2 years ago and has not traveled outside France since then. The only abnormality found in the baby at delivery is an anemia (12.3 g/dL hemoglobin) attributed to antiretroviral drugs toxicity (ARV given to mother?)
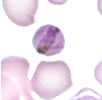
At 6 weeks post-delivery, the infant is brought in for a fever of one-day duration. She is found to have a temperature of 38.5°C and both hepatomegaly (3 cm) and splenomegaly (3 cm). Serologic tests for HBs and HCV are negative, and PCR, DNA and RNA for HIV are negative. More routine laboratory exams show hemoglobin 6.4 g/dL, platelets 122,000/µL, LDH 1080 IU/mL, and blood smears showing the following:
Blood smear 1

Blood smear 2

Blood smear 3
Question 1: What is your diagnosis?
No Malaria
That is incorrect. Please, try another answer.
Plasmodium falciparum
That is incorrect. Please, try another answer.
Plasmodium vivax
That is incorrect. Please, try another answer.
Plasmodium ovale
That is incorrect. Please, try another answer.
Plasmodium malariae
That is correct.
The most likely diagnosis, based on microscopy and clinical history is P. malariae. Note the typical microscopic characteristics: all stages of parasites present; band-form trophozoite (image 1); round, rosette-shaped schizont (image 2); and round gametocyte (image 3, at right). The microscopic diagnosis of P. malariae was confirmed by PCR. The parasitemia is 1.8%, which is high for P. malariae (note that in image 3, four parasites are crowded in a relatively small field). The mild or absent symptoms of malaria in the mother is compatible with P. malariae, a parasite that can persist for years, even a lifetime, with minimal symptoms. Plasmodium malariae is known to occur in DR Congo, where it is second in prevalence (by far) to P. falciparum.
Mixed infection (several Plasmodium species)
That is incorrect. Please, try another answer.
A transfusion of 125 mLs of blood is given to the child.
Question 2. What antimalarial drug would you administer to the infant?
Chloroquine
That is correct.
Chloroquine is the drug of choice for the treatment of Plasmodium malariae. P. malariae is chloroquine-sensitive, and additionally chloroquine is one of the safest antimalarial drugs available.
Doxycycline is contraindicated in young children, and halofantrine can have cardiotoxic effects.
Primaquine is not necessary because there are no dormant liver stages in this parasite species. At the usual doses, primaquine would have no effect on the blood stage parasites (it targets mainly the liver stage parasites, and the gametocytes).
Even in congenital malaria caused by P. vivax and P. ovale , which have liver stage parasites, primaquine treatment of the infant is not necessary because no liver stages are transmitted from the mother to the child.
Quinine-doxycycline
That is incorrect. Please, try another answer.
Mefloquine
That is incorrect. Please, try another answer.
Halofantrine
That is incorrect. Please, try another answer.
Primaquine
That is incorrect. Please, try another answer.
Following treatment with the orally administered antimalarial drug, parasitemia drops and the child becomes afebrile.
Question 3. What test(s) would you perform to confirm current infection of the mother?
Thin blood smear
That is correct.
All tests (with the exception maybe of serology) would be useful. The blood smears are the most practical tests for detecting an asymptomatic infection in the mother, with the thick smear being more sensitive. If both fail, and PCR is available, PCR would be even more sensitive than the thick smear. (When done correctly, PCR is the most sensitive and specific test for malaria detection and species identification.) Serology would not be useful in proving current infection.
Thick blood smear
That is correct.
All tests (with the exception maybe of serology) would be useful. The blood smears are the most practical tests for detecting an asymptomatic infection in the mother, with the thick smear being more sensitive. If both fail, and PCR is available, PCR would be even more sensitive than the thick smear. (When done correctly, PCR is the most sensitive and specific test for malaria detection and species identification.) Serology would not be useful in proving current infection.
PCR for malaria
That is correct.
All tests (with the exception maybe of serology) would be useful. The blood smears are the most practical tests for detecting an asymptomatic infection in the mother, with the thick smear being more sensitive. If both fail, and PCR is available, PCR would be even more sensitive than the thick smear. (When done correctly, PCR is the most sensitive and specific test for malaria detection and species identification.) Serology would not be useful in proving current infection.
Serology
That is incorrect. Please, try another answer.
A thick blood smear of the mother, taken 5 days after that of the infant, is indeed positive, while on the thin smear no parasites can be detected.
Main Points
Congenital malaria should be considered in febrile newborns and infants from women who could have been parasitemic during their pregnancy.
Malaria parasitemia during pregnancy can result because the mother became infected during her pregnancy, but it can also result from an infection acquired months or years before.
The woman in this case probably was infected in DR Congo more than 2 years before delivery. Untreated Plasmodium malariae infection can persist >40 years and remain relatively asymptomatic.
Plasmodium vivax and P. ovale can similarly cause malaria several months or years after the original infection, by reactivation of dormant liver stage parasites.
Diagnostic procedures for detecting active malaria infection are, in order of increasing sensitivity: thin blood smear, thick blood smear, and PCR. Serology does not detect active infection, but measures past exposure to malaria.
- Page last reviewed: October 7, 2015
- Page last updated: October 7, 2015
- Content source:


 ShareCompartir
ShareCompartir