CDC'S New High-impact Approach to HIV Prevention Funding for Health Departments Advancing the National HIV/AIDS Strategy
The Centers for Disease Control and Prevention (CDC) has announced a five-year HIV prevention funding opportunity for health departments in states, territories, and select cities. Providing funding to health departments has long been a central component of CDC’s HIV prevention strategy, and is CDC’s single largest investment in HIV prevention. CDC’s new funding opportunity represents a new direction designed to achieve a higher level of impact with every federal HIV prevention dollar.
CDC’s new approach features better geographic targeting of resources and a stronger focus on supporting the highest-impact prevention strategies. This approach embodies CDC’s commitment to High Impact Prevention—using scalable, cost-effective interventions with demonstrated potential to reduce new infections, in the right populations, to yield a major impact on the HIV epidemic. High Impact Prevention is essential to achieving the ambitious HIV prevention goals of the National HIV/AIDS Strategy, which was announced in 2010.
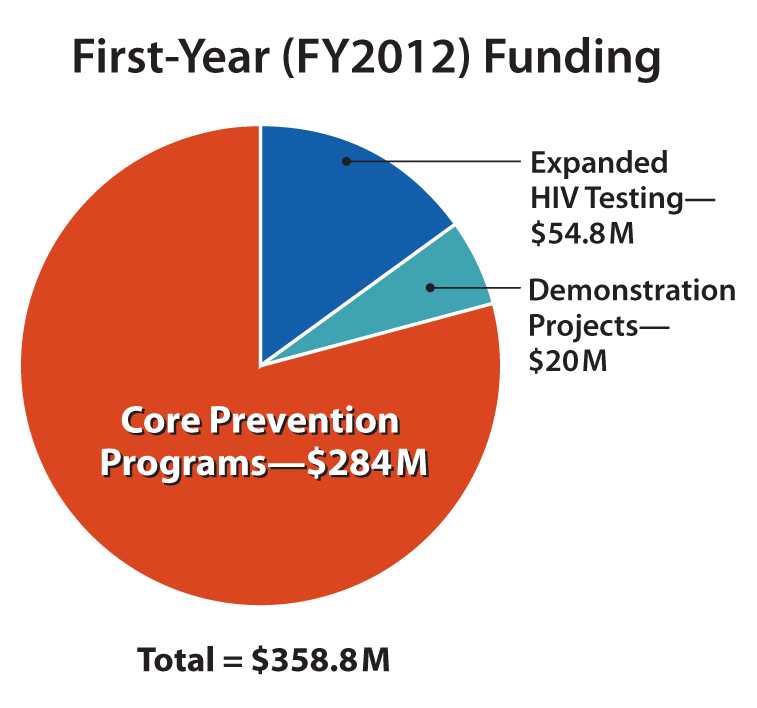
First-year (FY2012) awards under this funding opportunity will total $358.8 million, which is approximately level with current CDC HIV prevention funding for health departments. States, territories, and directly funded cities will apply for funding in September 2011, and the new funding cycle will begin in January 2012.
CDC’s new approach to HIV prevention funding for health departments was informed by input from many of CDC’s partners in the HIV community. In 2010, CDC consulted with and received input from several key partners, including the National Association of State and Territorial AIDS Directors (NASTAD), Urban Coalition for HIV/AIDS Prevention Services (UCHAPS), National Minority AIDS Council (NMAC), National Association of County and City Health Officials (NACCHO), The AIDS Institute, and local, state, and territorial health departments. Community input proved essential in developing several key elements of the funding opportunity, including a minimum funding level for all jurisdictions, the introduction of competitive funding for innovative demonstration projects, and the continuation of direct funding for heavily affected cities. CDC is confident that this approach reflects the input of many different parties and represents the best course of action.
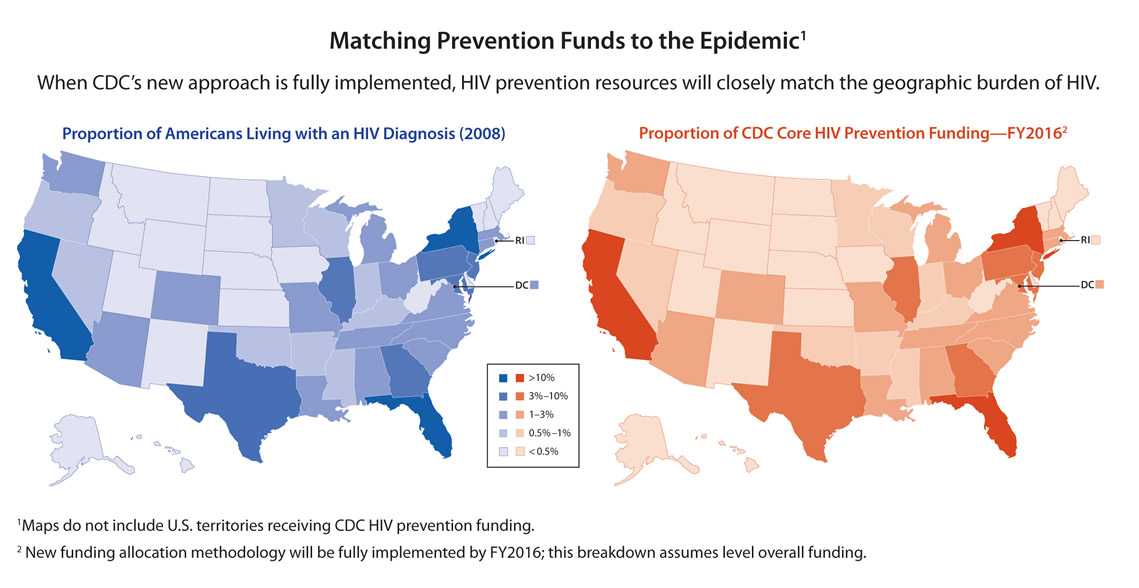
Better Matching Resources to the Geographic Burden of HIV
This health department funding opportunity employs a new method for allocating core HIV prevention resources to better match the geographic burden of the U.S. HIV epidemic today. Funding is apportioned to each state, territory, or directly funded city based on the number of people reported to be living with an HIV diagnosis in that jurisdiction in 2008 (the best measure of the HIV burden available in every U.S. jurisdiction). This approach, driven by the latest data, improves on prior health department funding allocations, which were based on AIDS cases earlier in the epidemic. (HIV data is a better indicator of the epidemic’s current burden than AIDS data, since less than half of all Americans living with HIV have progressed to AIDS.)
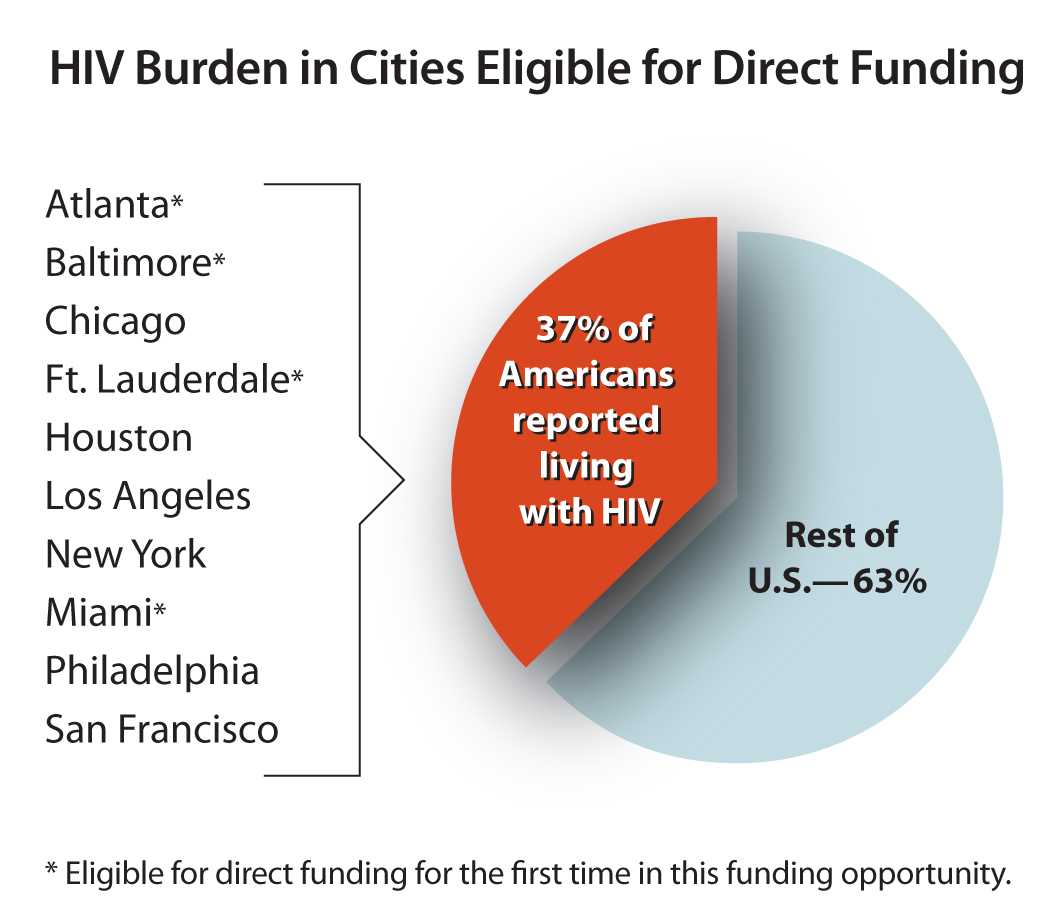
In addition, to ensure that funding reaches major urban areas where HIV is concentrated in the United States, the number of cities (metropolitan statistical areas) eligible for direct CDC funding will increase from six to ten. These ten cities account for approximately 37 percent of all Americans living with an HIV diagnosis.
While some health departments will see substantial changes in funding levels, the overall shift in funding for the entire funding opportunity is modest, representing approximately 10 percent of CDC’s core HIV prevention funding for health departments.
This relatively small change will have a major positive impact on the epidemic. Several areas with heavy HIV burdens will see needed increases in prevention funding, including many southern states and several major cities. While other areas will see decreases, CDC is taking steps to minimize disruptions due to shifts in funding. The new method for allocating resources incorporates a minimum funding level, to ensure that all jurisdictions, regardless of HIV burden, can continue to provide basic HIV prevention services. Funding shifts for all jurisdictions—both increases and decreases—will be phased in over five years, to allow health departments time to adjust strategies and infrastructure as necessary. In addition, no state’s funding will be reduced by more than one-quarter of its previous year’s budget. CDC will provide extensive technical support to assist health departments in navigating this transition (see Technical Assistance for Health Departments below).
Supported Activities: Prioritizing High Impact HIV Prevention
The funding opportunity also provides important new guidance to health departments about specific prevention strategies to prioritize. This guidance is intended to ensure that prevention funds are directed to the combinations of activities that are most likely to have a significant and lasting impact on the HIV epidemic.
CDC will fund health department HIV prevention activities in three categories:
-
Core prevention programs ($284M in FY2012):
The large majority of funding will support health departments’ core HIV prevention programs. At least three-quarters (75 percent) of this core funding must be directed to the following required activities, which have demonstrated potential to reduce new HIV infections:-
HIV testing: Approximately 240,000 Americans are unaware that they are living with HIV – by learning their status, they can take steps to protect their health and reduce the risk of transmission to others. Supported activities include:
- Routine opt-out testing of patients ages 13-64 in healthcare settings
- Targeted testing programs in non-healthcare settings, particularly venues most likely to reach individuals with undiagnosed infections
- Routine, early HIV screening for all pregnant women
- Screening for other STDs, hepatitis, and tuberculosis in conjunction with HIV testing
-
Comprehensive prevention with HIV-positive individuals:
- Linkages to care and treatment, and interventions to improve retention in care and treatment for people living with HIV (studies show that effective treatment can reduce the risk that an HIV-positive person will transmit the virus to others)
- Behavioral interventions and other risk-reduction services for HIV-positive individuals and their sexual or needle-sharing partners to reduce the likelihood of HIV transmission
- Interventions to prevent mother-to-child HIV transmission
- Referral to other medical and social services, such as substance abuse and mental health services
-
Condom distribution:
- Providing condoms to people living with HIV and those at highest risk of infection
-
Policy initiatives:
- Efforts to align structures, policies, and regulations to enable optimal HIV prevention, care, and treatment (e.g., addressing structural barriers to routine opt-out testing, or updating policies to facilitate sharing of surveillance data across health department programs)
- In addition, up to one-quarter (25 percent) of core prevention funding can be used to support other proven HIV activities, including:
-
Evidence-based interventions for high-risk populations:
- Individual and group-level interventions for HIV-negative people at highest risk of acquiring HIV
- Community-level interventions to reduce risk behaviors
- Syringe service programs, where allowable and in accordance with state and local laws
-
Social marketing, media, and mobilization:
- Marketing campaigns to educate and inform high-risk populations, healthcare providers, and other relevant audiences about HIV
- Using current technology (e.g., social networking sites, texting, and web applications) to reach the highest-risk populations
- Community mobilization to raise awareness, fight stigma, and encourage safe behaviors
-
PrEP and nPEP:
- Planning, education, personnel, and other support for pre-exposure prophylaxis (PrEP) for men who have sex with men (CDC funds may not be used for the purchase of PrEP medications). For more details on PrEP for men who have sex with men, see CDC’s interim guidance at cdc.gov/hiv/prevention/research/prep/index.html
- Non-occupational post-exposure prophylaxis (nPEP) for high-risk groups
- The core prevention work described above must be guided and supported by the following health department activities, which are also supported by CDC’s core prevention funding:
-
Jurisdictional HIV prevention planning:
- All health departments are required to have in place a prevention planning process, including an HIV prevention planning group (formerly HIV Community Planning Group) composed of a broad range of stakeholders across the continuum of HIV prevention, care and treatment services, and people living with HIV
- In order to streamline and strengthen the HIV planning process, CDC will soon introduce new HIV prevention planning guidelines for health departments and their partners. The new guidelines will be made available on CDC’s website
-
Capacity building and technical assistance:
- Capacity building assistance for local HIV prevention service providers
- Training for health department and healthcare facility staff, community-based organizations, and other partners
- Peer-to-peer consultation and technical assistance
-
Program planning, monitoring and evaluation, and quality assurance:
- Employing the most current epidemiological and surveillance data to guide planning
- Developing a comprehensive monitoring, evaluation, and quality assurance plan
-
HIV testing: Approximately 240,000 Americans are unaware that they are living with HIV – by learning their status, they can take steps to protect their health and reduce the risk of transmission to others. Supported activities include:
-
Expanded HIV testing for disproportionately affected populations ($54.8M in FY 2012):
The 36 jurisdictions with at least 3,000 African American and Hispanic residents living with an HIV diagnosis in 2008 are eligible for additional funding to expand access to HIV testing for populations disproportionately affected by HIV, including African Americans, Hispanics, men who have sex with men, and injection drug users. Supported activities include:- Routine, opt-out HIV screening in healthcare settings serving these populations (at least 70 percent of funding)
- Targeted HIV testing in non-healthcare venues frequented by high-risk individuals (up to 30 percent of funding)
This funding category builds on CDC’s recent Expanded Testing Initiative, which over a three-year period provided HIV testing services in 25 jurisdictions, diagnosing more than 18,000 individuals who were previously unaware of their HIV infection, 70 percent of whom were African American.
-
Demonstration projects ($20M in FY2012):
CDC’s health department HIV prevention funding opportunity includes a competitive category for demonstration projects designed to evaluate innovative approaches to HIV prevention. All jurisdictions can submit proposals for demonstration projects, and award decisions will be based on merit. Given the rapidly evolving nature of prevention science, health departments are invited to submit proposals for this category in the current funding cycle, 2013, and 2014.
Potential focus areas for demonstration projects include:
- Structural, behavioral, or biomedical interventions, individually or in combination, that will have high impact on reducing new HIV infections
- HIV testing approaches that increase identification of undiagnosed infections or improve cost effectiveness
- Enhanced linkage to and retention in medical care for individuals living with HIV
- Advanced use of technology (e.g., Internet services, electronic medical records) to prevent HIV infections
- Innovative use of CD4, viral load, and other surveillance data for HIV prevention
Technical Assistance for Health Departments
CDC recognizes that health departments already face tough choices about how to make the best use of limited funds. We believe that this new approach will increase the impact of prevention efforts on the national HIV epidemic, and are committed to helping our partners develop and implement the most effective HIV prevention strategies and navigate any changes introduced by this funding opportunity.
Health departments will have access to technical support through multiple channels, including a series of technical briefings; ongoing counsel from CDC project officers, Prevention Training Centers, and CDC-supported capacity-building providers on infrastructure, financial management, and implementation; and peer-to-peer support facilitated by NASTAD, UCHAPS, and other CDC partners. For health departments that see a decrease in funding based on the new approach, CDC will offer post-award site visits and more in-depth assistance to help them achieve the greatest impact from available funds.
- Page last reviewed: June 9, 2017
- Page last updated: August 24, 2017
- Content source: Division of HIV/AIDS Prevention, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, Centers for Disease Control and Prevention


 ShareCompartir
ShareCompartir