Kenya joins the world in ‘Closing the Immunization Gap’

The theme for this year’s World Immunization Week is “Closing the Immunization Gap” a slogan which challenges countries and public health practitioners around the world to address inequity in vaccination coverage.
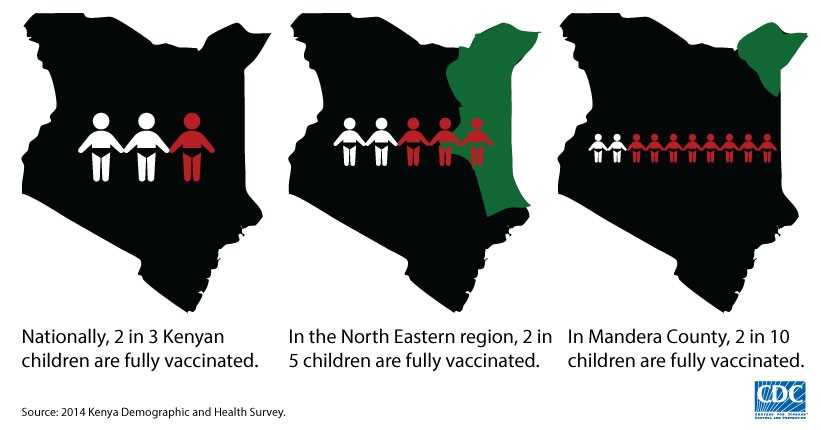
According to the 2014 Kenya Demographic and Health Survey (KDHS), about two of every three Kenyan children are considered “fully immunized.” While this is an important accomplishment, we recognize that our work is not complete until every child is fully immunized against preventable diseases. The KDHS illustrates clearly the challenge of immunization inequity: In contrast to the nation as a whole, only 41% of children in the North Eastern region are fully vaccinated, and within that region, only 27.7% of the children in Mandera County, the second poorest among Kenya’s 47 counties.
The Oxford English Dictionary defines “access” as “the right or opportunity to use or benefit from something.” To achieve equity in the delivery of immunization services, we need to improve our understanding of the factors that affect the accessibility of services and those that affect their utilization. While national statistics can paint a positive picture, we recognize that there are people whose access to care can be limited by geography, culture, awareness, conflict, economics, disability, policy, or attitudes. Capturing the many sides of access and utilization in a way that informs policy and the design of healthcare services that reach every child can be a challenge.
CDC’s Global Immunization Division (GID) has been exploring nomadic pastoralists’ access to services across Africa, and most recently in the North Eastern region of Kenya. Pastoralists are those whose household income is primarily based on raising livestock; nomadic pastoralists migrate with their animals seasonally in pursuit of grazing and water.
The traditional narrative adopted to explain low uptake of services by nomadic pastoralists is that they are “very poor,” they “move constantly” and thus are “hard to reach.” But this is the perspective of a healthcare system designed to deliver services in clinical settings or by means of “outreach” to well-identified and largely sedentary (though occasionally remote) communities.
Taking the nomadic pastoralists’ viewpoint lends a different perspective on both access and utilization. Proximity to good grazing and water for livestock is paramount to nomadic pastoralists; however, they must also settle near markets where they can sell their livestock and perishable dairy products. Thus, because animal husbandry is the main driver of their seasonal movements and settlement patterns, one must consider household decision-making around utilization of health services in the same context.
GID and CDC Kenya recently conducted a district-level survey in the North Eastern region of Kenya. Although we have not yet finished our analyses, the processes of designing and piloting the study were enlightening in and of themselves. Preliminary data challenge the long-held stereotypes of nomadic pastoralists as “poor” or “isolated.” Mobile phone coverage and the use of mobile money systems such as MPESA are high and continue to rise, even in areas with sporadic mobile network strength. In addition, we know from other countries, as well as in Kenya, that pastoralists are aware of the preventative value and economic benefits of vaccination for their livestock. Recognizing that pastoralists are able to “access” vaccines for their animals, by both passively accepting free vaccine and actively seeking vaccine and animal treatments for purchase, shifts the dialogue from geographic or economic “access” or “knowledge” to other factors that affect vaccine uptake among pastoralist children. Mothers may attribute illnesses to “God’s will,” or in the case of polio and some other diseases, [super]natural causes such as “wind”; in this way, understanding the local belief systems is of critical importance.
The context of mothers’ decision-making around immunization is also key. One woman explained that her child had never received a vaccine because she has “no time,” and “too many household chores.” As the main caregivers of small children, and generally the primary herders of smaller livestock like sheep and goats (and the producers of their dairy products), women have many responsibilities within the household, even when these are shared with co-wives or other community members.
To understand household-level decisions that affect utilization, we have to consider the trade-offs of competing demands on mothers’ time. While health facilities and animal markets are near to each other, the clinic schedule itself may constrain access for women whose priorities begin with childcare and extend through water collection, animal husbandry, etc. So when a mother travels to a clinic (perhaps at the expense of lost income from the market) to find it closed for an unscheduled “outreach day,” or stocked out of one or more vaccines, we can begin to see the features of a health system which can unintentionally create barriers to access and, therefore, limit utilization of services by those who need it most.
Through our research in Kenya, we hope to gain insights into the health-system factors, economic behaviors and networks, cultural beliefs, and household-level decision-making which affect access to and utilization of immunization services among pastoralists. Ultimately, we would like to use these data to effect change in service delivery to achieve equity by closing the immunization gap for all children.
- Page last reviewed: April 27, 2015
- Page last updated: April 27, 2015
- Content source:
Global Health
Notice: Linking to a non-federal site does not constitute an endorsement by HHS, CDC or any of its employees of the sponsors or the information and products presented on the site.


 ShareCompartir
ShareCompartir