Laboratory Testing
Epstein-Barr virus (EBV), also known as human herpesvirus 4, is a gamma herpes virus that occurs only in humans. Laboratory testing can help distinguish whether someone is susceptible to EBV infection or has a recent or past infection.
Healthcare providers can test for antibodies to the following EBV-associated antigens:
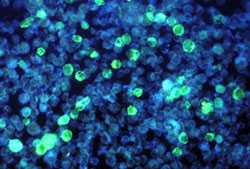
This photomicrograph depicts leukemia cells that contain Epstein-Barr virus using a FA staining technique.
- Viral capsid antigen (VCA)
- Anti-VCA IgM appears early in EBV infection and usually disappears within 4 to 6 weeks.
- Anti-VCA IgG appears in the acute phase of EBV infection, peaks at 2 to 4 weeks after onset, declines slightly then persists for the rest of a person’s life.
- Early antigen (EA)
Anti-EA IgG appears in the acute phase of illness and generally falls to undetectable levels after 3 to 6 months. In many people, detection of antibody to EA is a sign of active infection. However, 20% of healthy people may have antibodies against EA for years. - EBV nuclear antigen (EBNA)
Antibody to EBNA, determined by the standard immunofluorescent test, is not seen in the acute phase of EBV infection but slowly appears 2 to 4 months after onset of symptoms and persists for the rest of a person’s life. Other EBNA enzyme immunoassays may report false positive results. - Monospot test
The Monospot test is not recommended for general use. The antibodies detected by Monospot can be caused by conditions other than infectious mononucleosis. Moreover, studies have shown that the Monospot produces both false positive and false negative results. For example, the heterophile antibodies detected by Monospot are often not present in children with infectious mononucleosis. At best, the Monospot test may indicate that a person has a typical case of infectious mononucleosis, but does not confirm the presence of EBV infection.
Interpretation of EBV Antibody Tests
EBV antibody tests are not usually needed to diagnose infectious mononucleosis. However, specific antibody tests may be needed to identify the cause of illness in people who do not have a typical case of infectious mononucleosis or have other illnesses that can be caused by EBV infection. Symptoms of infectious mononucleosis generally resolve within 4 weeks. If a person is ill for more than 6 months and does not have a laboratory-confirmed diagnosis of EBV infection, other causes of chronic illness or chronic fatigue syndrome should be considered.
The interpretation of EBV antibody tests requires familiarity with these tests and access to the patient’s clinical information.
Interpretation of EBV antibody tests and diagnosis of EBV infection is summarized as follows:
- Susceptibility to infection
People are considered susceptible to EBV infection if they do not have antibodies to the VCA. - Primary (new or recent) infection
People are considered to have a primary EBV infection if they have anti-VCA IgM but do not have antibody to EBNA. Other results that strongly suggest a primary infection are a high or rising level of anti-VCA IgG and no antibody to EBNA after at least 4 weeks of illness. Resolution of the illness may occur before the diagnostic antibody levels appear. In rare cases, people with active EBV infections may not have detectable EBV-specific antibodies. - Past infection
The presence of antibodies to both VCA and EBNA suggests past infection (from several months to years earlier). Since over 90% of adults have been infected with EBV, most adults will show antibodies to EBV from infection years earlier. High or elevated antibody levels may be present for years and are not diagnostic of recent infection.
Testing paired acute- and convalescent-phase serum samples is not useful to distinguish between recent and past EBV infections. In most cases, the antibody response occurs rapidly during primary EBV infection. The clinical findings of infectious mononucleosis occur in conjunction with the appearance of IgG and IgM anti-VCA antibodies. However, the antibody pattern is not stable before symptoms appear.
- Page last reviewed: September 14, 2016
- Page last updated: January 7, 2014
- Content source:


 ShareCompartir
ShareCompartir