Statistics and Epidemiology
On This Page
Annual Cases of Ehrlichiosis in the United States
Ehrlichiosis was first recognized as a disease in the United States in the late 1980’s, but did not become a reportable disease until 1999. CDC compiles the number of cases reported by state health departments.
Both Ehrlichia chaffeensis and E. ewingii are causes of human illness in the United States, although the majority of reported cases are due to E. chaffeensis. During the early years of reporting, the disease caused by E. chaffeensis was commonly referred to as human monocytic ehrlichiosis (or HME). Compared to E. chaffeensis, very few E. ewingii cases have been documented in the published literature, and the disease was not considered separately reportable to CDC until 2008. Therefore, the national surveillance data for ehrlichiosis presented here reflects presumed infection due to E. chaffeensis,
The number of ehrlichiosis cases due to E. chaffeensis that have been reported to CDC has increased steadily since the disease became reportable, from 200 cases in 2000, to 961 cases in 2008. A decrease in the number of cases of ehrlichiosis was noted in 2010. The incidence (the number of cases for every million persons) of ehrlichiosis increased similarly, from less than 1 case per million persons in 2000 to 3.4 cases per million persons 2008, and has since decreased to 2.5 cases per million persons in 2010. Since becoming a reportable disease, the annual case fatality rate (i.e. the proportion of ehrlichiosis patients that died as a result of their infections) has declined.
Figure 1 – Number of U.S. E. chaffeensis cases* reported to CDC, 1994–2010
*Numbers presented here may differ from numbers presented in the MMWR Annual Summary of Notifiable Diseases. Data presented here are based on year of illness onset rather than reporting year.
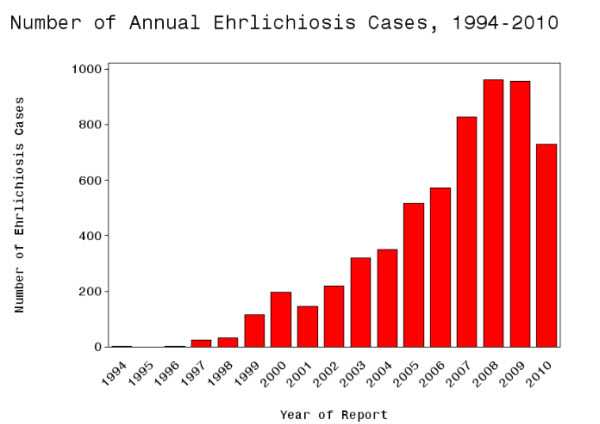
Data Table for Number of Annual Ehrlichiosis Cases, 1994 – 2010
The graph displays the number of human cases of ehrlichiosis cases reported to CDC annually from 1994 through 2010. Cases of ehrlichiosis have increased steadily from 200 cases in 2000, when the disease became nationally notifiable, to 961 cases in 2008. Cases decreased significantly in 2010 from 944 reported in 2009 to 740 reported in 2010.
Figure 2 – Proportion of U.S. E. chaffeensis cases reported to CDC with fatal outcome (case fatality rate), 2000–2010
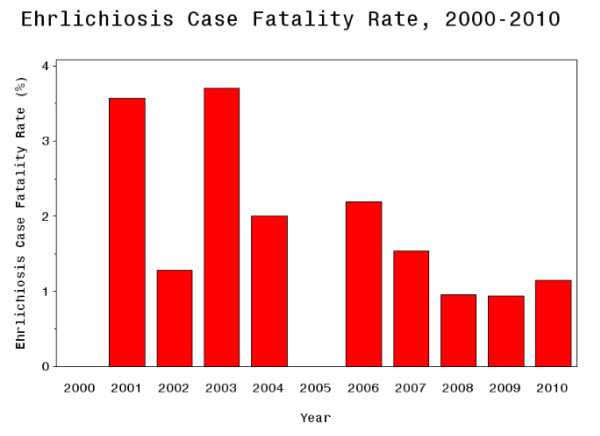
Data Table
This figure shows the proportion of fatal outcomes reported annually to CDC from 2000 through 2010. There were no fatalities reported in 2000 or 2005. Highest proportions of fatal cases were reported in 2001 and 2003, both of which reported over 3% fatality rates. In all other years case fatality rates hovered around 1—2%.
| Year | Fatality Rate |
|---|---|
| 2000 | No fatal cases reported |
| 2001 | 3.6% case fatality |
| 2002 | 1.3% case fatality |
| 2003 | 3.7% case fatality |
| 2004 | 2.0% case fatality |
| 2005 | No fatal cases reported |
| 2006 | 2.2% case fatality |
| 2007 | 1.5% case fatality |
| 2008 | 1.0% case fatality |
| 2009 | 0.9% case fatality |
| 2010 | 1.1% case fatality |
Geography
Ehrlichiosis is most frequently reported from the southeastern and south-central United States, from the eastern seaboard extending westward to Texas. The areas from which cases are reported correspond with the known geographic distribution of the lonestar tick (Amblyomma americanum), which is associated with transmission of both E. chaffeensis and E. ewingii. Three states (Oklahoma, Missouri, Arkansas) account for 30% of all reported E. chaffeensis infections. Occasionally, ehrlichiosis cases may be reported in other parts of the United States, including northern states where the lonestar tick is not commonly found. These cases may be due to patient travel to states with higher levels of disease, the presence of small populations of lonestar ticks outside commonly established areas, or the misdiagnosis of ehrlichiosis in patients actually infected with another tickborne disease, such as anaplasmosis or Rocky Mountain spotted fever.
Figure 3 – Annual reported incidence (per million population) for E. chaffeensis in the United States for 2010. (NN= Not notifiable)
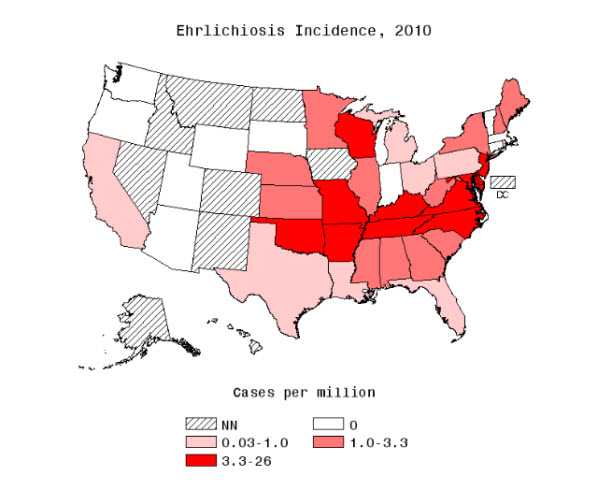
Data Table
This figure shows the incidence of ehrlichicosis cases by state in 2010 per million persons. Ehrlichiosis was not notifiable in Alaska, Colorado, the District of Columbia, Hawaii, Idaho, Iowa, Nevada, New Mexico, North Dakota or Montana. The incidence rate was zero for Arizona, Connecticut, Indiana, Massachusetts, Oregon, South Dakota, Utah, Vermont, Washington, and Wyoming. Incidence ranged between 0.03 to 1 case per million persons for California, Florida, Louisiana, Michigan, Ohio, Pennsylvania, Rhode Island and Texas. Annual incidence ranged from 1 to 3.3 cases per million persons in Alabama, Georgia, Illinois, Kansas, Maine, Minnesota, Mississippi, Nebraska, New Hampshire, New York, South Carolina and West Virginia. The highest incidence rates, ranging from 3.3 to 26 cases per million persons were found in Arkansas, Delaware, Kentucky, Maryland, Missouri, New Jersey, North Carolina, Oklahoma, Tennessee, Virginia, and Wisconsin.
Seasonality
Although cases of ehrlichiosis can occur during any month of the year, the majority of cases reported to the CDC have an illness onset during the summer months and a peak in cases typically occurs in the months of June and July. This period is the season for increased numbers of adult and nymphal lonestar ticks, which are the primary life stages of ticks that bite humans and if infected can transmit disease.
Figure 4 – Proportion of E. chaffeensis cases reported to CDC by month of onset, 2010.
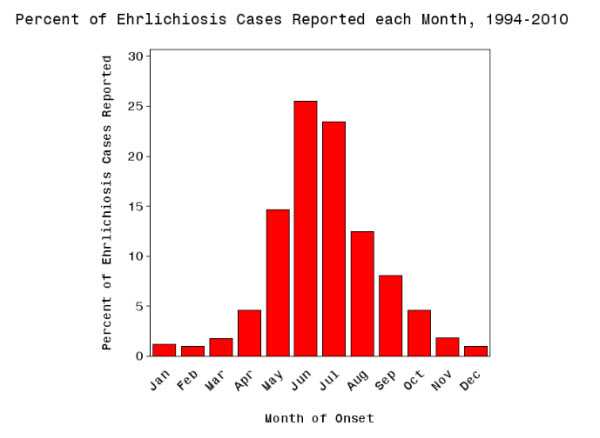
Data Table
This figure shows the percent of cases reported from 1994 through 2010 by month of onset to give the seasonality of cases. There are cases reported in each month of the year, however most are reported between May and August. More than 25% of cases are reported in June.
Persons at Risk
The frequency of reported cases of ehrlichiosis is highest among males and people over 50 years of age. A compromised immune system (such as may occur through cancer treatments, advanced human immunodeficiency virus infection, prior organ transplants, or some medications) may increase the risk of severe outcome. Individuals who reside near or spend time in wooded areas or areas with high grass may be at increased risk for infection.
Figure 5 – Average annual incidence of ehrlichiosis by age group, 2010
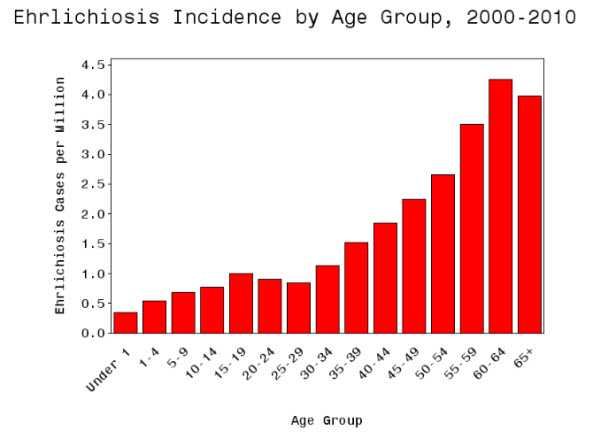
Data Table
This figure shows the average annual incidence of ehrlichiosis per million persons by age groups for 2000 through 2010. The graph shows that cases have been reported in every age group with increased incidence as age increases. The highest rate of incidence, more than 4 cases per million persons, is seen in persons ages 60-64 years.
E. ewingii Surveillance
E. ewingii infections are impossible to distinguish from E. chaffeensis infections based on clinical signs alone, and some proportion of cases currently reported as E. chaffeensis infection may actually be due to E. ewingii. There is no currently available serologic test that can distinguish these agents, and surveillance for E. ewingii is currently based on detection of the organism through molecular-based diagnostic tests. Beginning in 2008, a new separate reporting category was established for E. ewingii infection. A total of 28 cases of E. ewingii were reported to CDC from 2008–2010.
Other Ehrlichiosis, Undetermined
This reporting category reflects cases that showed clinical and laboratory signs consistent with either an ehrlichiosis or anaplasmosis infection, but which could not be attributed to a specific organism due to the limitations of diagnostic test results. This category is also used to report new cases of human illness attributed to other Ehrlichia species previously unknown to cause human infections. In 2009, an Ehrlichia species that appears to be closely related to Ehrlichia muris, and which has been provisionally called E. muris-like (or EML), was identified as a cause of human illness for the first time in the United States. Since its initial identification, at least six persons residing in Wisconsin and Minnesota have been confirmed with infection with the EML organism.
Further Reading
Dahlgren FS, Mandel EJ, Krebs JW, Massung RF, McQuiston JH. Increasing incidence of Ehrlichia chaffeensis and Anaplasma phagocytophilum in the United States, 2000–2007. Am J Trop Med Hyg (85)2011,124
Demma LJ, Holman RC, McQuiston JH, Krebs JW, Swerdlow DL. Epidemiology of human ehrlichiosis and anaplasmosis in the United States, 2001–2002. Am J Trop Med Hyg (73)2005,400
CDC. Anaplasmosis and ehrlichiosis – Maine, 2008. MMWR Morb Mort Wkly Rep (58)2009,1033
Diagnosis and Management of Tickborne Rickettsial Diseases: Rocky Mountain Spotted Fever and Other Spotted Fever Group Rickettsioses, Ehrlichioses, and Anaplasmosis — United States. MMWR Recomm Rep (65)2016,1-44.
- Page last reviewed: January 25, 2016
- Page last updated: January 25, 2016
- Content source:


 ShareCompartir
ShareCompartir