
DPDx is an education resource designed for health professionals and laboratory scientists. For an overview including prevention and control visit www.cdc.gov/malaria/.
Malaria
[Plasmodium falciparum] [Plasmodium knowlesi] [Plasmodium malariae] [Plasmodium ovale] [Plasmodium vivax]
Diagnostic Findings
Microscopy
Microscopy (morphologic analysis) continues to be the "gold standard" for malaria diagnosis. Parasites may be visualized on both thick and thin blood smears stained with Giemsa, Wright, or Wright-Giemsa stains. Giemsa is the preferred stain, as it allows for detection of certain morphologic features (e.g. Schüffner’s dots, Maurer’s clefts, etc.) that may not be seen with the other two. Ideally, the thick smears are used to detect the presence of parasites while the thin smears are used for species-level identification. Quantification may be done on both thick and thin smears.
| Plasmodium species | Stages found in blood | Appearance of Erythrocyte (RBC) | Appearance of Parasite |
|---|---|---|---|
| P. falciparum | Ring | normal; multiple infection of RBC more common than in other species; Maurer's clefts (under certain staining conditions) | delicate cytoplasm; 1 to 2 small chromatin dots; occasional appliqué (accolé) forms |
| Trophozoite | normal; rarely, Maurer's clefts (under certain staining conditions) | seldom seen in peripheral blood; compact cytoplasm; dark pigment | |
| Schizont | normal; rarely, Maurer's clefts (under certain staining conditions) | seldom seen in peripheral blood; mature = 8 to 24 small merozoites; dark pigment, clumped in one mass | |
| Gametocyte | distorted by parasite | crescent or sausage shape; chromatin in a single mass (macrogametocyte) or diffuse (microgametocyte); dark pigment mass | |
| P. vivax | Ring | normal to 1.25x, round; occasionally fine Schüffner's dots; multiple infection of RBC not uncommon | large cytoplasm with occasional pseudopods; large chromatin dot |
| Trophozoite | enlarged 1.5 to 2x; may be distorted; fine Schüffner's dots | large amoeboid cytoplasm; large chromatin; fine, yellowish-brown pigment | |
| Schizont | enlarged 1.5 to 2x; may be distorted; fine Schüffner's dots |
large, may almost fill RBC; mature = 12 to 24 merozoites; yellowish-brown, coalesced pigment | |
| Gametocyte | enlarged 1.5 to 2x; may be distorted; fine Schüffner's dots | round to oval; compact; may almost fill RBC; chromatin compact, eccentric (macrogametocyte) or diffuse (microgametocyte); scattered brown pigment | |
| P. ovale | Ring | normal to 1.25x, round to oval; occasionally Schüffner's dots; occasionally fimbriated; multiple infection of RBC not uncommon | sturdy cytoplasm; large chromatin |
| Trophozoite | normal to 1.25x; round to oval; some fimbriated; Schüffner's dots | compact with large chromatin; dark-brown pigment | |
| Schizont | normal to 1.25x, round to oval, some fimbriated, Schüffner's dots | mature = 6 to 14 merozoites with large nuclei, clustered around mass of dark-brown pigment | |
| Gametocyte | normal to 1.25x; round to oval, some fimbriated; Schüffner's dots | round to oval; compact; may almost fill RBC; chromatin compact, eccentric (macrogametocyte) or more diffuse (microgametocyte); scattered brown pigment | |
| P. malariae | Ring | normal to 0.75x | sturdy cytoplasm; large chromatin |
| Trophozoite | normal to 0.75x; rarely, Ziemann's stippling (under certain staining conditions) | compact cytoplasm; large chromatin; occasional band forms; coarse, dark-brown pigment | |
| Schizont | normal to 0.75x; rarely, Ziemann's stippling (under certain staining conditions) | mature = 6 to 12 merozoites with large nuclei, clustered around mass of coarse, dark-brown pigment; occasional rosettes | |
| Gametocyte | normal to 0.75x; rarely, Ziemann's stippling (under certain staining conditions) | round to oval; compact; may almost fill RBC; chromatin compact, eccentric (macrogametocyte) or more diffuse (microgametocyte); scattered brown pigment | |
| P. knowlesi | Ring | normal to 0.75x; multiple infection not uncommon. | delicate cytoplasm; 1 to 2 prominent chromatin dots; occasional appliqué (accolé) forms |
| Trophozoite | normal to 0.75x; rarely, Sinton and Mulligan's stippling (under certain staining conditions) | compact cytoplasm; large chromatin; occasional band forms; coarse, dark-brown pigment | |
| Schizont | normal to 0.75x; rarely, Sinton and Mulligan's stippling (under certain staining conditions) | mature = up to 16 merozoites with large nuclei, clustered around mass of coarse, dark-brown pigment; occasional rosettes; mature merozoites appear segmented | |
| Gametocyte | normal to 0.75x; rarely, Sinton and Mulligan's stippling (under certain staining conditions) | round to oval; compact; may almost fill RBC; chromatin compact, eccentric (macrogametocyte) or more diffuse (microgametocyte); scattered brown pigment |
Molecular Diagnosis
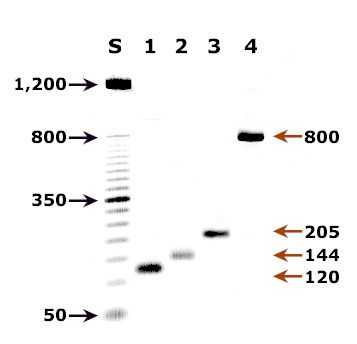
Agarose gel (2%) analysis of a PCR diagnostic test for species-specific detection of Plasmodium DNA.
Morphologic characteristics of malaria parasites can determine a parasite species, however, microscopists may occasionally fail to differentiate between species in cases where morphologic characteristics overlap (especially Plasmodium vivax and P. ovale), as well as in cases where parasite morphology has been altered by drug treatment or improper storage of the sample. In such cases, the Plasmodium species can be determined by using confirmatory molecular diagnostic tests. In addition, molecular tests such as PCR can detect parasites in specimens where the parasitemia may be below the detectable level of blood film examination. The methods currently used at CDC are described below.
Species-specific PCR diagnosis of malaria
Plasmodium genomic DNA is extracted from 200 µl whole blood using the QIAamp Blood Kit (Cat. No. 29106; Qiagen Inc., Chatsworth, CA.) or a similar product that can yield the comparable concentration of genomic DNA from the same volume of blood.
Detection and identification of Plasmodium to the species level is done with a real-time PCR assay as described by Rougemont et al 2004. This is a dual duplex assay that detects P. falciparum and P. vivax in one reaction, and P. malariae and P. ovale in a parallel reaction, using species-specific TaqMan probes. In cases where infection by more than one Plasmodium species is suspected, there is an option to use a conventional nested PCR assay (Snounou el al, 1993) that has an improved resolution of mixed infection compared to the real-time PCR assay.
Agarose gel (2%) analysis of a PCR diagnostic test for species-specific detection of Plasmodium DNA. PCR was performed using nested primers of Snounou et al.1
- Lane S: Molecular base pair standard (50-bp ladder). Black arrows show the size of standard bands.
- Lane 1: The red arrow shows the diagnostic band for P. vivax (size: 120 bp).
- Lane 2: The red arrow shows the diagnostic band for P. malariae (size: 144 bp).
- Lane 3: The red arrow shows the diagnostic band for P. falciparum (size: 205 bp).
- Lane 4: The red arrow shows the diagnostic band for P. ovale (size: 800 bp).
Reference:
Mathieu Rougemont, Madeleine Van Saanen, Roland Sahli, Hans Peter Hinrikson, Jacques Bille and Katia Jaton. Detection of Four Plasmodium Species in Blood from Humans by 18S rRNA Gene Subunit-Based and Species-Specific Real-Time PCR Assays. J. Clin. Microbiol. 2004, 42(12):5636.
Snounou G, Viriyakosol S, Zhu XP, et al. High sensitivity detection of human malaria parasites by the use of nested polymerase chain reaction. Mol Biochem Parasitol 1993;61:315-320.
Antibody Detection
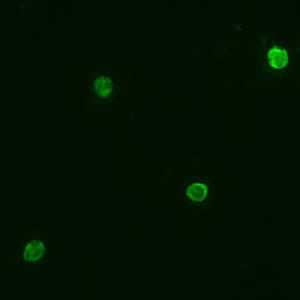
Positive IFA result with P. malariae schizont antigen.
Malaria antibody detection for clinical diagnosis is performed using the indirect fluorescent antibody (IFA) test. The IFA procedure can be used as a diagnostic tool to determine if a patient has been infected with Plasmodium. Because of the time required for development of antibody and also the persistence of antibodies, serologic testing is not practical for routine diagnosis of acute malaria. However, antibody detection may be useful for:
- screening blood donors involved in cases of transfusion-induced malaria when the donor's parasitemia may be below the detectable level of blood film examination
- testing a patient who has been recently treated for malaria but in whom the diagnosis is questioned
Species-specific testing is available for the four human species: P. falciparum, P. vivax, P. malariae, and P. ovale. Cross reactions often occur between Plasmodium species and Babesia species. Blood stage Plasmodium species schizonts (meronts) are used as antigen. The patient's serum is exposed to the organisms; homologous antibody, if present, attaches to the antigen, forming an antigen-antibody (Ag-Ab) complex. Fluorescein-labeled antihuman antibody is then added, which attaches to the patient's malaria-specific antibodies. When examined with a fluorescence microscope, a positive reaction is when the parasites fluoresce an apple green color.
Reference:
Sulzer AJ, and Wilson M. The fluorescent antibody test for malaria. Crit Rev Clin Lab Sci 1971;2:601-609.
Antigen Detection
In addition to microscopy and molecular methods, there are methods for detecting malaria parasites on the basis of antigens or enzymatic activities associated with the parasites. These methods are often packaged as individual test kits called rapid diagnostic tests or RDTs.
These methods include, among others:
- detection of an antigen (histidine rich protein-2, HRP-2) associated with malaria parasites (P. falciparum)
- detection of a Plasmodium specific aldolase
- detection of a Plasmodium associated lactate dehydrogenase (pLDH) either through its enzymatic activity or by immunoassay
There is currently only one RDT licensed for use in the United States. For additional information visit http://www.cdc.gov/malaria/diagnosis_treatment/rdt.html
 ShareCompartir
ShareCompartir
 Preparation of Blood Smears [PDF, 2 Pages, 77 KB]
Preparation of Blood Smears [PDF, 2 Pages, 77 KB] Staining for Malaria Parasites [PDF, 2 Pages, 44 KB]
Staining for Malaria Parasites [PDF, 2 Pages, 44 KB] Laboratory diagnosis of Plasmodium falciparum [PDF, 4 pages, 127 KB]
Laboratory diagnosis of Plasmodium falciparum [PDF, 4 pages, 127 KB] Laboratory Diagnosis of Plasmodium vivax [PDF, 4 pages, 166 KB]
Laboratory Diagnosis of Plasmodium vivax [PDF, 4 pages, 166 KB] Laboratory Diagnosis of Plasmodium ovale [PDF, 4 pages, 165 KB]
Laboratory Diagnosis of Plasmodium ovale [PDF, 4 pages, 165 KB]  Laboratory Diagnosis of Plasmodium malariae [PDF, 4 pages, 149 KB]
Laboratory Diagnosis of Plasmodium malariae [PDF, 4 pages, 149 KB] Comparison of the Plasmodium Species Which Cause Human Malaria [PDF, 2 pages, 28 KB]
Comparison of the Plasmodium Species Which Cause Human Malaria [PDF, 2 pages, 28 KB] Plasmodium spp. Blood Stage Parasites, Thin Blood Smears [PDF, 4 pages, 512 KB]
Plasmodium spp. Blood Stage Parasites, Thin Blood Smears [PDF, 4 pages, 512 KB]  Plasmodium spp. Blood Stage Parasites, Thick Blood Smears [PDF, 2 pages, 938 KB]
Plasmodium spp. Blood Stage Parasites, Thick Blood Smears [PDF, 2 pages, 938 KB] Calculating Percent Parasitemia and Life Cycle of Plasmodium Species [PDF, 2 pages, 80 KB]
Calculating Percent Parasitemia and Life Cycle of Plasmodium Species [PDF, 2 pages, 80 KB]

