For Clinicians
Español: Para médicos
Conjunctivitis can result from many causes, including viruses, bacteria, allergens, contact lens use chemicals, fungi, and certain diseases.
Schools should allow infected children to remain in school once any indicated therapy is implemented, except when viral or bacterial conjunctivitis is accompanied by systemic signs of illness. However, infected students should refrain from attending school if their behavior is such that they cannot avoid close contact with other students. [1]
Viral Conjunctivitis

Colorized transmission electron micrograph of adenovirus.
(CDC Public Health Image Library)
The following viruses can cause vial conjunctivitis, with adenoviruses being one of the most common causes:
- Adenoviruses
- Rubella virus
- Rubeola (measles) virus
- Herpesviruses, including
- Herpes simplex virus
- Varicella-zoster virus, which also causes chickenpox and shingles
- Epstein-Barr virus, which also causes infectious mononucleosis (mono)
- Picornaviruses, such as coxsackievirus A24 and enterovirus 70 (which has caused outbreaks in other countries)
Viral conjunctivitis is highly contagious. Most viruses that cause conjunctivitis spread through hand-to-eye contact by hands or objects that are contaminated with the infectious virus. Having contact with infectious tears, eye discharge, fecal matter, or respiratory discharges can contaminate hands. Viral conjunctivitis can also spread by large respiratory tract droplets.
Depending on the cause of viral conjunctivitis, some patients may have additional symptoms or conditions, such as the following:
- Common cold, flu, or other respiratory infection
- Pharyngoconjunctivial fever — a syndrome that can produce conjunctivitis as well as a fever and sore throat, and is most commonly caused by infection with adenovirus serotypes 3, 4, and 7
- Epidemic keratoconjunctivitis — a more severe type of conjunctivitis, commonly caused by infection with adenovirus serotypes 8, 19, and 37
- Acute hemorrhagic conjunctivitis — a type of conjunctivitis that is often associated with large epidemics worldwide, especially in the tropical and subtropical regions. The viruses most commonly associated with it include enterovirus 70, coxsackievirus A24, and adenoviruses.
- Herpetic keratoconjunctivitis — a type of conjunctivitis associated with herpes simplex virus and blister-like lesions on the skin; it may affect only one eye
- Rubella and rubeola (measles) — conjunctivitis can occur with these viral rash illnesses which are usually accompanied by rash, fever, and cough
Bacterial Conjunctivitis

This illustration shows Streptococcus pneumoniae, one common cause of bacterial conjunctivitis.
Acute bacterial conjunctivitis is the most common form of bacterial conjunctivitis in outpatient healthcare settings. [2] The bacteria that most commonly cause bacterial conjunctivitis in the United States are
- Staphylococcus aureus
- Haemophilus influenzae
- Streptococcus pneumoniae
- Moraxella catarrhalis
Bacterial conjunctivitis can spread from person to person, from hand-to-eye contact or via eye contact with contaminated objects. Alternatively, changes in the usual bacteria that live on the conjunctiva can cause conjunctivitis. Bacteria can also spread by large respiratory tract droplets.
Topical antimicrobial therapy is indicated for bacterial conjunctivitis, which is usually distinguished by a purulent exudate.
Depending on the cause of bacterial conjunctivitis, some patients may have additional symptoms or conditions, such as the following:
Hyperacute bacterial conjunctivitis
- A more severe type of conjunctivitis that develops rapidly and can lead to corneal perforation
- Often accompanied by eyelid swelling, pain, and decreased vision
- Involves a large amount of thick, purulent (pus) discharge that returns even after wiping it away from the eye(s)
- Often caused by Neisseria gonorrhoeae in sexually active adults
- Can lead to vision loss if not treated promptly by an eye doctor [2]
Chronic bacterial conjunctivitis
- Defined as symptoms lasting for at least 4 weeks
- Often happens along with blepharitis, inflammation of the eyelid lid, which can cause flaky debris and warmth along the lid
- People with this condition should see an eye doctor [3]
Chlamydial conjunctivitis
- In neonates
- Can occur in infants born to mothers with Chlamydia trachomatis
- It is called ophthalmia neonatorum in the first 4 weeks of life
- Usually symptoms develop 5 to 12 days after birth
- Neonates with chlamydia conjunctivitis also often have chlamydial infection elsewhere in their bodies (e.g., lungs, nasopharynx). Approximately 50% of infants with pneumonia have a history of chlamydia conjunctivitis
- Often presents with mucopurulent or bloody discharge, marked swelling with red, thickened, and friable conjunctivae, and a pseudomembrane may form
- Among sexually active people
- Acute disease is commonly unilateral with hyperemia and purulent discharge and caused by Chlamydia trachomatis subtypes D-K
- Many patients will have a more mild prolonged course
- Most cases have a genital infection caused by chlamydia just prior to or at the same time
- Trachoma
- A chronic follicular conjunctivitis caused by Chlamydia trachomatis subtypes A through C, which causes scarring of the eyelid, conjunctiva, and cornea
- A leading global cause of preventable blindness
- Transmitted from person to person through contact with discharge from the eyes or nose of an infected person, through shared items, or by flies
- Repeat infections occur in children younger than 10 years of age
- Common where access to basic hygiene is poor
Learn more about trachoma and other hygiene-related diseases.
Gonococcal conjunctivitis
- Common cause of hyperacute conjunctivitis in neonates and sexually active people
- Includes red eyes, thick pus in the eyes, and swelling of the eyelids
- In newborns, it usually presents in the first 5 days of life and can be associated with bacteremia and meningitis
- Prophylaxis with erythromycin ophthalmic ointment is currently recommended by the U.S. Preventive Services Task Force immediately after birth and is legally mandated in most states
- Gonococcal conjunctivitis in adults is uncommon and treatment data are limited; an infectious disease practitioner should be consulted
Allergic Conjunctivitis
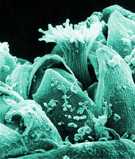
Scanning electron micrograph of an Ambrosia trifida plant, more commonly known as ragweed.
(CDC Public Health Image Library)
Allergic conjunctivitis is common in people who have other signs of allergic disease, such as hay fever, asthma, and eczema. It is caused by the body’s reaction to certain substances to which it is allergic, such as
- Pollen from trees, plants, grasses, and weeds
- Dust mites
- Animal dander
- Molds
- Contact lenses and lens solution
- Cosmetics
Related Pages
Footnotes
1 American Academy of Pediatrics. Recommendations for care of children in special circumstances. In: Kimberlin DW, Brady MT, Jackson MA, Long SS, eds. Red Book: 2015 Report of the Committee on Infectious Diseases. 30th ed. Elk Grove Village, IL: American Academy of Pediatrics; 2015.
2 Crounau H, Kankanala RR, Mauger T. Diagnosis and management of red eye in primary care. Am Fam Physician. 2010;81:137-44.
3 Høvding G. Acute bacterial conjunctivitis. Acta Ophthalmol. 2008;86(1):5–17.
- Page last reviewed: October 16, 2017
- Page last updated: October 16, 2017
- Content source:


 ShareCompartir
ShareCompartir