ART and Intracytoplasmic Sperm Injection (ICSI) in the United States
Key Findings: Use of Intracytoplasmic Sperm Injection (ICSI) in the United States
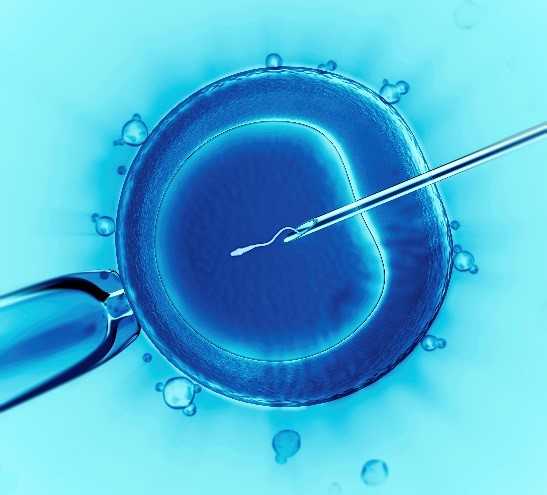 Intracytoplasmic sperm injection (ICSI) is a technique used during in vitro fertilization (IVF) where a single sperm is injected directly into the egg for the purpose of fertilization. During conventional IVF, the egg is placed in a culture dish with many sperm and fertilization occurs when one sperm penetrates the egg naturally. According to the American Society for Reproductive Medicine, ICSI is a safe and effective procedure for couples with male factor infertility and can improve the chance of fertilization for couples with poor fertilization in a previous IVF cycle.
Intracytoplasmic sperm injection (ICSI) is a technique used during in vitro fertilization (IVF) where a single sperm is injected directly into the egg for the purpose of fertilization. During conventional IVF, the egg is placed in a culture dish with many sperm and fertilization occurs when one sperm penetrates the egg naturally. According to the American Society for Reproductive Medicine, ICSI is a safe and effective procedure for couples with male factor infertility and can improve the chance of fertilization for couples with poor fertilization in a previous IVF cycle.
Use of ICSI for couples with male factor infertility has increased over time since the technique was introduced in the early 1990s. However, ICSI is also increasingly used in patients without male factor infertility where the procedure has not been shown to improve clinical outcomes. Findings from some but not all studies suggest that ICSI is associated with an increased risk for chromosomal abnormalities, autism, intellectual disabilities, and birth defects compared with conventional IVF. These increased risks may also be due to the effects of subfertility. ICSI also adds to the cost of an IVF cycle, making it more expensive than conventional IVF. Data from CDC’s National ART Surveillance System were used to study national trends in the use of ICSI for couples with and without male factor infertility during 1996-2012. Reproductive outcomes for cycles using conventional IVF and those using ICSI among patients with male factor infertility and among patients with non-male factor infertility during 2008-2012 were also compared. These findings provide important information on the benefits and risks of ICSI.
Has the use of ICSI increased over time?
- For cycles with male factor infertility, ICSI use increased from 76.3% in 1996 to 93.3% in 2012.
- For cycles without male factor infertility, ICSI use increased from 15.4% in 1996 to 66.9% in 2012.
- Similar increases were found for selected non-male factor infertility indications, including unexplained infertility, maternal age 38 years or older, low oocyte yield, having 2 or more prior assisted reproductive technology cycles and no prior live births, and use of preimplantation genetic testing. ICSI use also increased in the absence of any of these indications, suggesting that other reasons may be influencing the clinical decision to use ICSI.
What were the reproductive outcomes of ICSI cycles compared with conventional IVF?
- For cycles with a diagnosis of male factor infertility, the likelihood of cycle cancellation between egg retrieval and embryo transfer (a surrogate measure of failed fertilization) was markedly decreased for cycles where ICSI was used, compared with those using conventional IVF, confirming that ICSI increases the chances of fertilization for couples with male factor infertility. There was no difference in cycle cancellation for couples without male factor infertility.
- For cycles with a male factor infertility diagnosis, ICSI use was associated with reduced rates of implantation and multiple births, compared with conventional IVF. However, rates of pregnancy, miscarriage, and live birth were not different for cycles using ICSI versus conventional IVF.
- For cycles without male factor infertility, ICSI use was associated with decreased rates of implantation, pregnancy, live birth, and multiple live births compared with conventional IVF.
More about these findings
- Overall, use of ICSI did not improve reproductive outcomes, regardless of whether male factor infertility was present. This may be due to poorer quality embryos resulting from cycles where ICSI was used because the procedure bypasses natural barriers to fertilization. It is also possible that characteristics of patients who were candidates for ICSI weren’t captured such as poor egg or sperm quality; differences in these factors could explain the findings.
- The primary limitation of our study is that we were unable to directly assess rates of fertilization, where ICSI is expected to be advantageous over conventional IVF.
Key Findings Reference
- Boulet SL, Mehta A, Kissin DM, Warner L, Kawwass JF, Jamieson DJ. Trends in use of and reproductive outcomes associated with intracytoplasmic sperm injection. JAMA. 2015;313(3):255-63. http://www.ncbi.nlm.nih.gov/pubmed/25602996
- Page last reviewed: October 12, 2016
- Page last updated: October 12, 2016
- Content source:
- Maintained By:


 ShareCompartir
ShareCompartir